Introduction
Urinary incontinence (UI) is the involuntary leakage of urine. It affects around 15% of the general population, most common in the elderly, and is more common in females (male: female 1:3)
UI can be categorised into various subtypes, all of which have different underlying causes and management options:
- Stress incontinence
- Urge incontinence
- Mixed incontinence
- Overflow incontinence
- Continuous incontinence
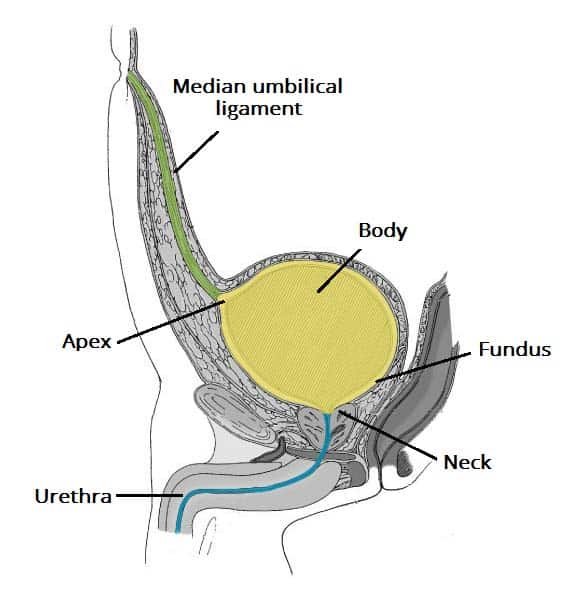
Figure 1 – Sagittal section of the male pelvis, demonstrating the anatomical features of the bladder
Pathophysiology
Stress UI
Stress UI is urine leakage occurring when the intra-abdominal pressure exceeds the urethral pressure, such as coughing, straining, laughing, or lifting. The impaired urethral support is most often due to weakness of the pelvic floor muscle.
It is most commonly seen post-partum, due to the damage occurring to the pelvic floor muscles, weakening the urethral sphincter. Other risk factors include constipation (due to recurrent straining), obesity, post-menopausal, or pelvic surgery (e.g. TURP, resulting in external sphincter damage)
Urge UI
Urge UI describes an overactive bladder (detrusor hyperactivity), which leads to uninhibited bladder contraction, leading to a rise in intravesical pressure and subsequent leakage of urine.
Such overactive bladder may be due to neurogenic causes (such as a previous stroke), infection, malignancy, or idiopathic. Medication, such as cholinesterase inhibitors, can also result in urge UI.
Mixed UI
Mixed UI is a combination of stress UI and urge UI.
Overflow UI
Overflow UI is normally a complication of chronic urinary retention, whereby the progressive stretching of the bladder wall leads to damage to the efferent fibres of the sacral reflex and loss of bladder sensation.
As the bladder fills with urine, it becomes grossly distended however intravesicular pressure builds, leading to a constant dribbling of urine.
The most common cause is from prostatic hyperplasia, however other causes include spinal cord injury or congenital defects.
Continuous UI
Continuous UI is the constant leakage of urine, meaning the patient is wet all the time. This is typically due to anatomical abnormality (such as ectopic ureter) or bladder fistulae (e.g. vesicovaginal fistula), however may also be due to severe overflow incontinence.
Clinical Features
A detailed clinical history can allow many cases of UI to be categorised on the first visit. Other symptoms (e.g. dysuria or haematuria), precipitating factors, past medical and surgical history, and drug history will all aid in patient work-up.
Patients should be asked to keep bladder diaries, which can aid in the delineation of the underlying cause. QoL questionnaires (such as ICIQ, BFLUTS, I‑QOL) can aid in quantifying severity of the condition.
Examination can aid in assessment of potential underlying causes, such as an enlarged prostate, prolapse, or any fistula opening.
Investigations
All patients should have a midstream urine dipstick performed, assessing for evidence of infection or haematuria. Post-void bladder scans should also be performed routinely, especially in those suspected of overflow UI.
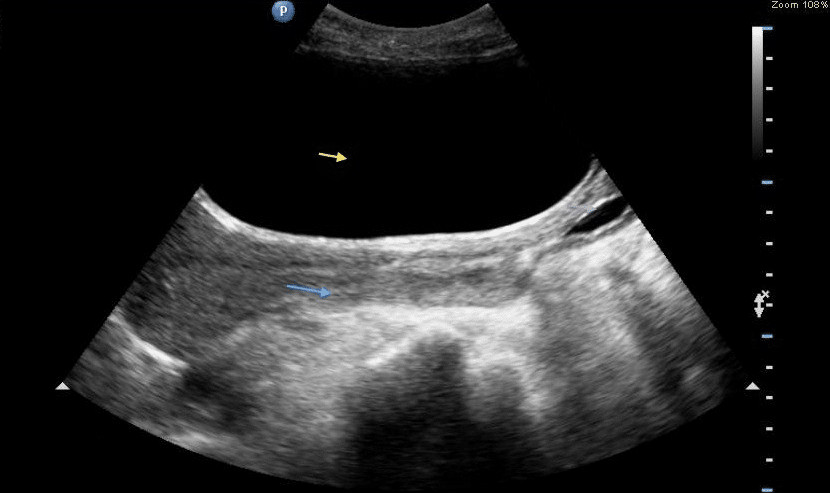
Figure 2 – Ultrasound bladder scan, showing an enlarged bladder in urinary retention (yellow arrow)
Further Investigations
For those with unclear aetiology, urodynamic assessment* can be a useful adjunct in the assessment of UI cases. Intravesicular and intra-abdominal pressures are measured, allowing detrusor muscle pressure to be calculated; any hyperactivity of the bladder muscle wall may suggest an urge UI.
Outflow urodynamics can then also be performed, to measure detrusor muscle activity against urine flow rate. For example, the presence of high intra-vesicular pressure with poor urine flow would suggest an overflow UI.
Other investigations that may be used include cystoscopy, intravenous urogram, vaginal speculum examination, or MRI imaging
*Urodynamic testing is not routinely preformed before starting conservative management, and is only considered in those with suspected detrusor over-activity, symptoms suggestive of voiding dysfunction, or have had previous surgery for stress UI
Management
Non-surgical therapy should be attempted initially when managing UI. Lifestyle advice is given to most patients presenting with UI, including weight loss, reducing caffeine intake, avoid drinking either excessive fluid volumes each day, and smoking cessation
Conservative Management
For stress UI (or mixed UI), initial management is supervised pelvic floor muscle training (PFMT), which should ideally last for at least 3 months. For those with limited response to PFMT (especially those unsuitable for surgery), often duloxetine (a serotonin–norepinephrine reuptake inhibitor) can be trialled, working to cause stronger urethral contractions.
For urge UI, anti-muscarinic drugs can be trialled, such as oxybutynin or tolterodine, acting to inhibit the detrusor contraction. Bladder training should also be offered, ensuring the patient continues this for a minimum of 6 weeks.
Surgical Management
For those remaining symptomatic despite conservative management, surgical options can be considered. There are multiple possible surgical management options, which one will be used depends on the initial diagnosis.
For urge UI, options include botulinum toxin A injections, percutaneous sacral nerve stimulation, augmentation cystoplasty (whereby a detubularised segment of bowel is inserted into the bladder wall to increase bladder capacity), or urinary diversion via ileal conduit.
For stress UI, options include tension-free vaginal tape, open colposuspension (involving elevation of the bladder neck and urethra through a lower abdominal incision), intramural bulking agents, or an artificial urinary sphincter
Key Points
- Urinary incontinence is the involuntary leakage of urine
- Subtypes are stress incontinence, urge incontinence, mixed incontinence, overflow incontinence, and continuous incontinence
- Suitable investigations and management are dependent on the suspected underlying cause
