Introduction
Haemorrhoids are defined as an abnormal swelling or enlargement of the anal vascular cushions.
The anal vascular cushions act to assist the anal sphincter in maintaining continence. There are three vascular cushions in the anus, positioned at the 3-, 7-, and 11- o’clock positions (when looked at with the patient in the lithotomy position, i.e. anterior is 12 o’clock).
When these cushions become abnormally enlarged, they can cause symptoms and become pathological, termed haemorrhoids.
The prevalence of haemorrhoids varies, mainly due to wrong attribution of anorectal symptoms, however it is estimated that around 4% of individuals in the USA have symptomatic haemorrhoids to varying degree. They have a prevalence peak at age 45-65yrs.

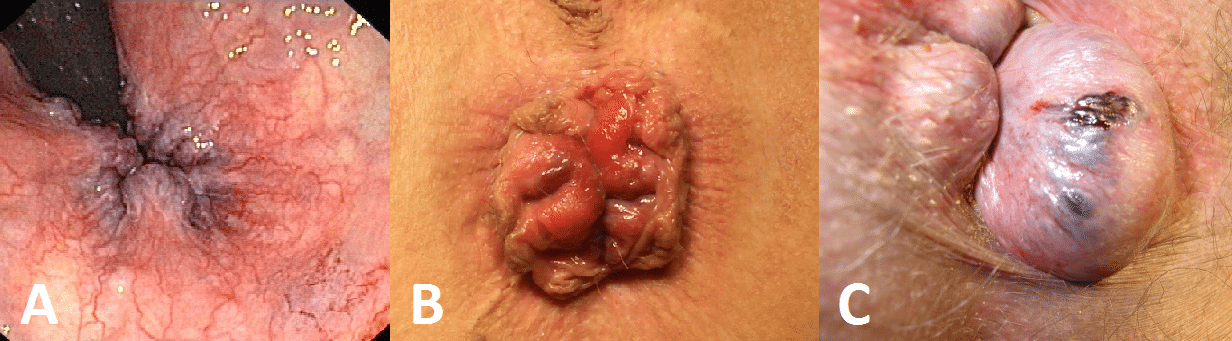
Figure 1 – Haemorrhoids located in the 3, 7, and 11 o’clock positions
Haemorrhoids are classified according to their size:
| Classification | Description |
| 1st Degree | Remain in the rectum |
| 2nd Degree | Prolapse through the anus on defecation but spontaneously reduce |
| 3rd Degree | Prolapse through the anus on defecation but require digital reduction |
| 4th Degree | Remain persistently prolapsed |
Table 1 – Classification of Haemorrhoids
Risk Factors
The main risk factors for the development of haemorrhoids are excessive straining (from chronic constipation), increasing age, and raised intra-abdominal pressure (such as pregnancy, chronic cough, or ascites).
Other less common risk factors include pelvic or abdominal masses, family history, cardiac failure, or portal hypertension.
Clinical Features
Haemorrhoids typically present with painless bright red rectal bleeding, commonly after defecation and often seen either on paper or covering the pan. Importantly, blood is seen on the surface of the stool, not mixed in.
Other symptoms include pruritus (due to chronic mucus discharge and irritation), rectal fullness or an anal lump, and soiling (due to impaired continence or mucus discharge).
Large prolapsed haemorrhoids can thrombose. These are very painful and these patients frequently present acutely to Emergency Departments
Examination will usually be normal unless the haemorrhoids have prolapsed. A thrombosed prolapsed haemorrhoid will present as a purple/blue, oedematous, tense, and tender perianal mass (Fig. 2C).
Differential Diagnosis
It is important to exclude other cause of rectal bleeding such as malignancy, inflammatory bowel disease, or diverticular disease.
Other perianal differentials to consider include fissure-in-ano, a perianal abscess, or fistula-in-ano. So-called “external piles” are usually just simple skin tags or “sentinel piles” from a fissure-in-ano.
Investigations
Proctoscopy is typically performed to confirm the diagnosis. Any significant or prolonged bleeding or signs of anaemia would warrant a full blood count and a clotting screen.
A colonoscopy is often advised (especially if complicated haemorrhoids) to exclude any concurrent anorectal pathology, before any surgical intervention for haemorrhoids is started.
Management
Nearly all haemorrhoids can be managed conservatively, especially if uncomplicated.
Ensure to provide lifestyle advice, such as increasing daily fibre and fluid intake to avoid constipation, prescribing laxatives if necessary. Topical analgesia (such as lignocaine gel) may also be required for pain relief; avoid oral opioid analgesia as this can compound any constipation and worsen symptoms.
For thrombosed haemorrhoids, sitting on ice packs and topical lidocaine gel can be useful for pain relief. In most situations, haemorrhoidectomy for a thrombosed haemorrhoid is not recommended, due to failure to resolve symptoms and higher risk of complications.
Symptomatic 1st and 2nd degree haemorrhoids can be treated with rubber-band ligation (RBL). This involves the haemorrhoid being drawn into the end of a suction gun and a rubber band placed over the neck of the haemorrhoid. This can be done either in a clinic setting or in theatre.
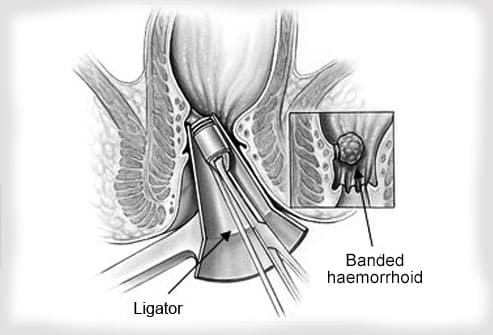
Figure 3 – Illustration of Rubber-Band Ligation (RBL) of haemorrhoids
Surgical
Haemorrhoidal artery ligation (HAL, also termed Transanal Haemorrhoid Dearterialisation (THD)) is one surgical option for 2nd or 3rd degree haemorrhoids, with equivocal effectiveness to other interventions. The main vessel supplying the haemorrhoid is identified through Doppler and then tied off, such that the haemorrhoid infarcts and falls off.
For 3rd degree and 4th degree haemorrhoids, another surgical option available is haemorrhoidectomy, especially those not suitable for banding or injection; the haemorrhoidal tissue is excised*, ensuring internal sphincter muscle remains. The exposed tissue can be either left open (e.g. a Milligan Morgan technique) or the mucosa closed (either sutured or stapled, Fig. 4).
The main complications following surgical interventions for haemorrhoids include recurrence, anal stricturing, or faecal incontinence.
*There should be sufficient skin bridges between excised areas to limit stricturing during healing – if the haemorrhoids are extensive and circumferential, haemorrhoidectomies may need to be carried out in multiple staged procedures
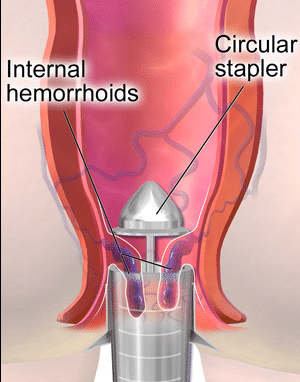
Figure 4 – Illustration showing principles of stapled haemorrhoidectomy
Key Points
- Haemorrhoids are defined as an abnormal swelling or enlargement of the anal vascular cushions
- There are four subtypes of haemorrhoids, classified from 1st to 4th degree
- Haemorrhoids typically present with painless bright red bleeding
- Haemorrhoids can be managed either conservatively or with surgical intervention if required