Introduction
Chronic mesenteric ischaemia (CMI) is caused by a reduced blood supply to the bowel which gradually deteriorates over time as a result of atherosclerosis in the coeliac trunk, superior mesenteric artery (SMA), and/or inferior mesenteric artery (IMA).
Chronic mesenteric ischaemia occurs mostly in those >60yrs and is more common in female patients. Patients with atherosclerotic disease in the mesenteric vessels are often asymptomatic, due to collateralisation, and as such this atherosclerosis is typically asymptomatic.
In this article, we shall look at the causes, clinical features and management of the patient with chronic mesenteric ischaemia.
Pathophysiology
The gradual build-up of atherosclerotic plaque within the mesenteric vessels narrows the lumen, impairing blood flow to the supplied viscera, resulting in an inadequate blood supply to the bowel.
Collateral blood supply means that commonly at least two of the Coeliac, SMA, and IMA must be affected for the patient to be symptomatic, most likely with at least one vessel occluded.
At rest patients are typically asymptomatic, however any increased demand on the blood supply, i.e. after eating, or a reduction in overall blood volume, such as severe haemorrhage, will exacerbate symptoms.
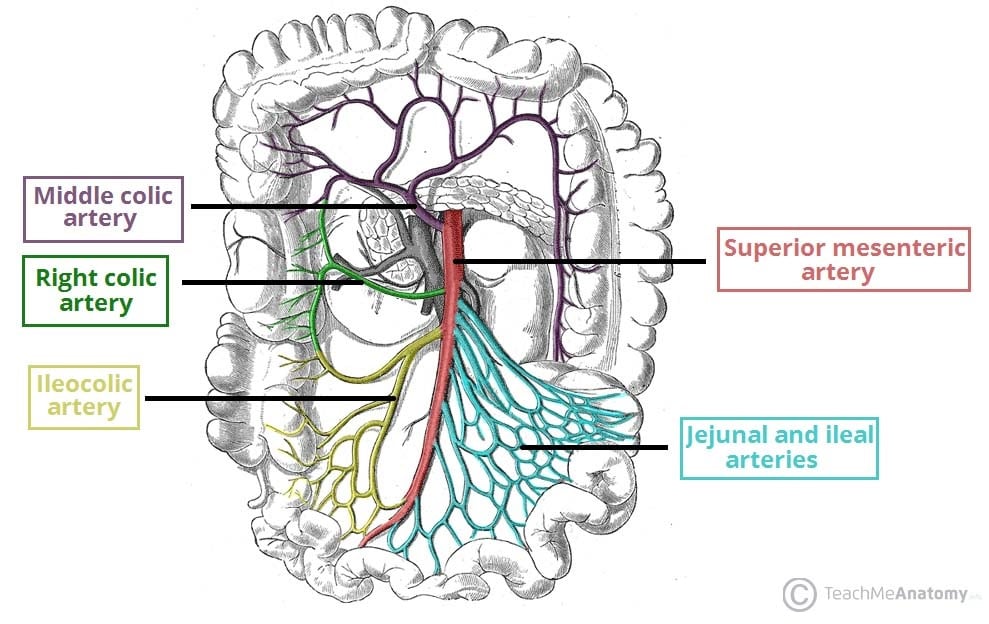
Figure 1 – The arterial supply from the superior mesenteric artery to the midgut
Risk Factors
The main risk factors for chronic mesenteric ischaemia are smoking, hypertension, diabetes mellitus, and hypercholesterolemia.
Clinical Features
The classical set of symptoms associated with chronic mesenteric ischaemia are:
- Postprandial pain – classically occurring around 10mins-4hrs after eating*
- Weight loss – a combination of decreased calorie intake and malabsorption
- Concurrent vascular co-morbidities, e.g. previous MI, stroke, or PVD
Other less specific symptoms may include change in bowel habit (typically loose), nausea, and vomiting. Examination findings are often non specific; evidence of malnutrition/cachexia, generalised abdominal tenderness, and abdominal bruits may be present.
*This may be associated with a fear of eating (sitophobia), as eating becomes linked to pain
Differential Diagnosis
Often a patient has undergone several other investigations for other pathologies before the diagnosis of chronic mesenteric ischaemia is reached.
Possible differentials for the chronic non-specific abdominal pain may include chronic pancreatitis, gallstone pathology, peptic ulcer disease, or upper GI malignancy
Investigations
Blood tests will routinely be normal, yet typically routine bloods (including FBC, U&Es, and LFTs) will have been performed prior to the diagnosis of chronic mesenteric ischaemia being reached. Electrolytes such as magnesium and calcium should be checked due to malnutrition.
Anaemia may be confounding symptoms and cardiovascular risk profile factors, such as lipids profile or blood glucose level, may be abnormal.
CT angiography is the diagnostic test of choice*, providing good anatomical views of all vessels and can help gauge any intervention required;
*Catheter angiography previously was the gold standard imaging modality but is now used less frequently
Management
Initial management for patients with chronic mesenteric ischaemia is to modify risk factors, especially smoking cessation, and commencing anti-platelet and statin therapy to minimise disease progression.
Following conservative management, both endovascular and open procedures may be available. Due to the general nutritional status of the patient and complexity of open surgery, endovascular treatment is often preferred, and are therefore managed jointly between interventional radiologists and vascular surgeons.
Surgical Treatment
Surgical intervention is warranted in severe disease, progressive disease, or presence of debilitating symptoms (including signs of weight loss or malabsorption).
The ultimate decision about which approach to take will depend on the location and severity of the disease, alongside patient choice and co-morbidities:
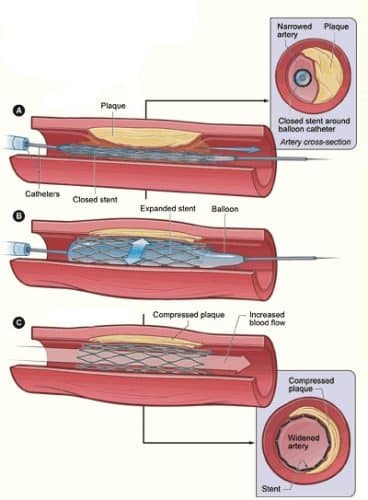
- Endovascular procedures (more common) – consists of mesenteric angioplasty with stenting
- Open procedures (less common) – either an endartectomy or a bypass procedure
Mesenteric Angioplasty
Mesenteric angioplasty is performed percutaneously, through either the femoral artery or brachial/axillary artery, allowing a catheter to be passed to the appropriate vessel under radiological guidance.
Once the affected region is identified, a small balloon is expanded to dilate the vessel, and stenting typically undertaken to maintain vessel patency.
Such procedures provide a shorter hospital stay with faster mobilisation for the patient. However, if the stent occludes at any point, the patient can develop acute mesenteric ischaemia.
Complications
The main complications of chronic mesenteric ischaemia are bowel infarction or malabsorption. Many patients will also have concurrent cardiovascular disease which will also require suitable medical management and optimisation.
Prognosis after intervention is good, with comparable results in terms of symptom relief between open surgery and endovascular methods.
Key Points
- Chronic mesenteric ischaemia is reduced blood supply to the bowel, often associated in patients with concurrent cardiovascular disease
- Patients will complain of post-prandial pain and weight loss, in an otherwise unremarkable examination
- Definitive diagnosis often comes from CT angiography
- Patients with chronic mesenteric ischaemia can be treated with endovascular or open procedures, if deemed suitable, and should have any cardiovascular risk factors addressed accordingly