Introduction
Acute kidney injury (AKI) is a common, but often predictable and avoidable complication post-operatively. It should be considered a significant medical condition that warrants early diagnosis, investigation and management.
Definition
Acute kidney injury can be defined (as per KDIGO and RIFLE criteria) as any of the following:
- ≥50% rise in serum creatinine from baseline within last 7 days
- Increase in serum creatinine by ≥26.5μmol/l within 48 hours
- Urine output <0.5mls/kg/hour (oliguria) for more than 6 hours
The severity of AKI can be classified by creatinine level, relative to baseline:
- Stage 1 = 1.5-1.9 times the baseline
- Stage 2 = 2-2.9 times the baseline
- Stage 3 = >3 times the baseline
Causes
The causes of acute kidney injury can be categorised into pre-, intra- or post- renal causes.
Perioperatively, pre-renal causes are the most common but it is still important to consider and exclude the other causes (most common causes have been placed in bold)
Pre-renal
- Sepsis
- Dehydration (including pre-operative NBM or bowel preparation)
- Haemorrhage
- Cardiac failure
- Liver failure (causing a hepatorenal syndrome)
- Renal artery stenosis
Important to remember that any intra-operative damage to the renal arteries can also cause pre-renal AKI. This is common in vascular procedures, such as from accidental graft occlusion, endovascular emboli, or proximal aortic clamp applied for too long.

Figure 2 – Pathological kidney specimen from a patient with AKI, showing necrosis of the cortex visible
Intra-renal
- Nephrotoxins, such as NSAIDs, ACEi (or ARBs), antibiotics (such as aminoglycosides), or chemotherapy (such as cisplatin)
- Parenchymal Disease, such as glomerulonephritides, acute tubulointerstitial nephritis, rhabdomyolysis, Haemolytic Uraemic Syndrome (HUS), or multiple myeloma
Post-renal
- Ureteric
- Retroperitoneal fibrosis
- Bilateral renal stones
- Tumours (either mural or extra-mural)
- Bladder
- Acute urinary retention
- Blocked catheter
- Urethral
- Prostatic enlargement (BPH or malignancy)
- Renal stones
Investigations
Examine the patient and assess their fluid status, alongside a bladder scan for any evidence of retention, before reviewing the drug chart for any nephrotoxins that could be causing or confounding the condition.
A urine dip will help in identifying a potential underlying cause. Initial bloods should be taken alongside U&Es, including FBC, CRP, LFTs, and Ca2+. A blood gas if useful in severe cases to ensure no significant acid-base disturbance secondary to renal dysfunction has occurred.
Urine Dipstick and Differentiating Causes of AKI
A urine dip can aid in differentiating between pre-renal and intrinsic causes of AKI
Urine specific gravity and osmolality values will be higher in pre-renal causes, whilst urine Na excretion will be lower, due to the kidney actively conserving Na and water in pre-renal cases, compared to intrinsic causes.
Any glomerulonephritis will show high levels of blood and protein.
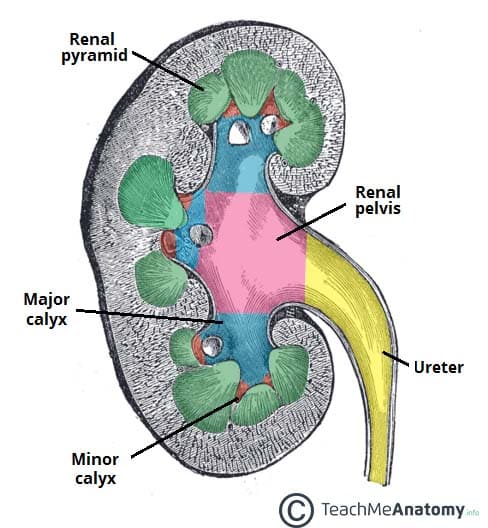
Imaging
An ultrasound scan of the kidneys, ureters and bladder is required in severe cases of AKI, especially if there is no response to initial management, in order to evaluate for any obstructive causes.
Any hydronephrosis present can indicate a potential obstructive pathology in the urinary tract that can be addressed accordingly if the underlying cause of the AKI
Management
Acute kidney injury should be viewed as a medical emergency and treatment should be instigated in a timely fashion. The condition is associated with worse morbidity and mortality, hence should be managed promptly.
If the patient is critically unwell, resuscitate the patient as necessary and inform your senior, before attempting to treat the underlying cause.
Fluid Status
Assess the patient’s hydration status, looking predominantly for signs of dehydration, such as dry mucous membranes, increased capillary refill time, reduced skin turgor, tachycardia, or (in severe cases) hypotension.
If suspected of pre-renal AKI, give a fluid bolus (between 250-500mL, depending on the patient) and re-assess their fluid status after 10-15 minutes, monitoring the urine output after the bolus. Give repeat fluid boluses until the patient is euvolaemic, before prescribing maintenance fluids if required.
Ongoing Monitoring
Re-assess the patient clinically on a regular basis and ensure they have regular observations*.
Start monitoring urine output, starting a fluid balance chart and consider catheterising the patient to permit more accurate assessment. Regular blood tests (especially U&Es) are required to monitor the progression of serum creatinine.
In those that do not respond to fluid therapy, consider intrinsic or post-renal aetiology as the underlying cause for the condition and manage accordingly
*If the patient is fluid overloaded and in AKI (for example, the cause is cardiac failure), begin daily weight monitoring and obtain specialist input
Drug Rationalisation
Medications can both affect and be affected by the kidneys, so its important that medications are reviewed in cases of AKI
- Drugs to be potentially stopped:
- ACEi and ARBs
- NSAIDs
- Aminoglycoside antibiotics
- Potassium-sparing diuretics (due to increased risk of hyperkalaemia)
- Drugs to be altered or reduced:
- Metformin (risk of lactic acidosis)
- Diuretics (in cases of intra-vascular fluid depletion)
- Low-molecular weight heparin
Key Points
- AKI is associated with worse patient outcomes and needs to be managed promptly
- Causes can be divided into pre-renal, intrinsic, and post-renal causes
- Fluid status, bladder scan, urine dip, routine bloods, and ultrasound scans all form part of the work-up of cases of AKI
- Ensure to treat the underlying condition and monitor regularly for response