Introduction
Distal femur fractures are fractures extending from the distal metaphyseal-diaphyseal junction of the femur to the articular surface of the femoral condyles.
They account for around 3-6% of femur fractures. They occur both in younger patients (as the result of high energy trauma) or in older patients (from low energy trauma as a pathological fracture secondary to osteoporosis or malignancy).
There is also an increasing number of whom have a distal femur fracture related to a knee replacement (known as a peri-prosthetic fracture).
Classification
The classification is commonly used to classify distal femur fractures into extra-articular (type A), partial articular (type B), and complete articular (type C).
Partial articular fractures can be further classified into sagittal fractures of lateral condyle, sagittal fractures of medial condyle, and coronal fractures.
Hoffa Fracture
A Hoffa fracture is a specific type of type B articular distal femoral fracture in which there is a fracture of the posterior aspect of the femoral condyles in the coronal plane. Hoffa fragments are more commonly unicondylar affecting the lateral femoral condyle.
Clinical Features
Patients commonly present following a fall or a traumatic injury. They will complain of severe pain in the distal thigh and an inability to weight bear.
On examination, there may be an obvious deformity, with associated swelling and ecchymosis of the distal thigh. If the fracture extends intra-articular, then a knee effusion may be present (from haemarthrosis).
It is also important to look for any evidence of an open fracture, which occurs in 5-10% of cases. Ensure to perform a full neurovascular examination of the lower limbs to identify any potential vascular or peripheral nerve injuries.
Differential Diagnosis
As most cases present following a fall or trauma, differentials include tibial plateau fractures, haemarthrosis, or tibial shaft fractures.
Investigations
Patients presenting following a major trauma should be investigated and managed as per the ATLS protocol.
Urgent bloods, including a coagulation and Group and Save, should be sent. If a pathological cause is suspected, further work-up bloods, such as a serum calcium and myeloma screen, may be warranted.
Imaging
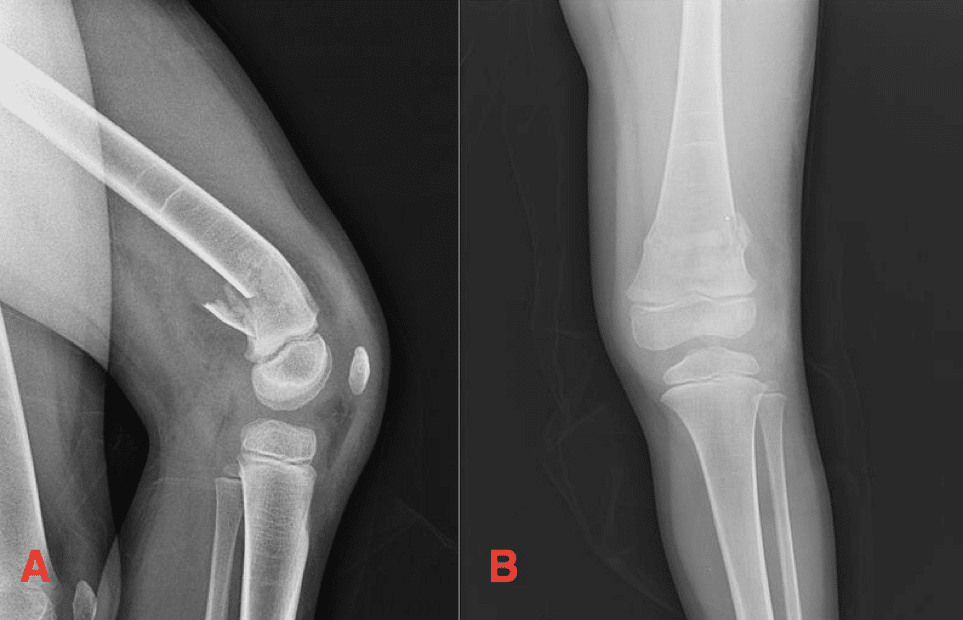
Antero-posterior (AP) and lateral plain film radiographs* of the knee and entire femur should be requested in suspected cases (Fig. 2)
If there is any intra-articular extension, then CT imaging is helpful to evaluate intra-articular involvement and assist in operative planning.
*Lateral views are essential to ensure a Hoffa fracture is not missed
Management
Any significant malalignment of the fracture will warrant initial realignment in A&E (with analgesia / sedation) and then immobilised using skin traction. Any evidence of an open fracture needs to be managed accordingly.
The majority of distal femur fractures are managed surgically. Non-operative management requires a long period of immobilisation and non-weight bearing, however is sometimes indicated for fractures with minimal displacement in a non-ambulatory or very co-morbid patient.
Surgical Management
The mainstay of surgical management for distal femur fractures is retrograde nailing or open reduction internal fixation (ORIF).
Retrograde intramedullary nailing is indicated in more proximal extra-articular fractures or simple intra-articular fractures, whilst an ORIF with a distal femoral plate is often indicated for more distal fractures or complex intra-articular fractures
In certain cases, external fixation may be used in severe comminuted or open fractures.
Peri-prosthetic Fractures
The management of a peri-prosthetic distal femur fracture is more complex, and may require intramedullary nailing, open reduction internal fixation, revision to a long stem prosthesis, or a distal femoral replacement.
Open reduction internal fixation is often the preferred method in the presence of an intact and stable prosthesis, while long stem revision or distal femoral replacement is more commonly employed when the femoral component is loose.
Complications
Complications following a distal femur fracture include malunion (more common for fractures that have been plated), non-union (can occur in up to 19%, most common in the metaphyseal area), and secondary osteoarthritis, especially those with intraarticular extension of the fracture.
Key Points
- Distal femur fractures are fractures extending from the distal metaphyseal-diaphyseal junction of the femur to the articular surface of the femoral condyles.
- They can occur in both younger patients (from high energy trauma) and in older patients (as frailty or pathological fractures)
- Antero-posterior and lateral plain film radiographs of the knee and entire femur should be requested in suspected cases
- The mainstay of management for distal femur fractures is retrograde nailing or open reduction internal fixation (ORIF)