Introduction
Epistaxis refers to bleeding from the nose. In the vast majority of cases they will terminate with simple manoeuvres and minimal intervention. However, in a small proportion of patients, epistaxis can lead to significant haemorrhage warranting urgent intervention.
Epistaxis can be occur from:
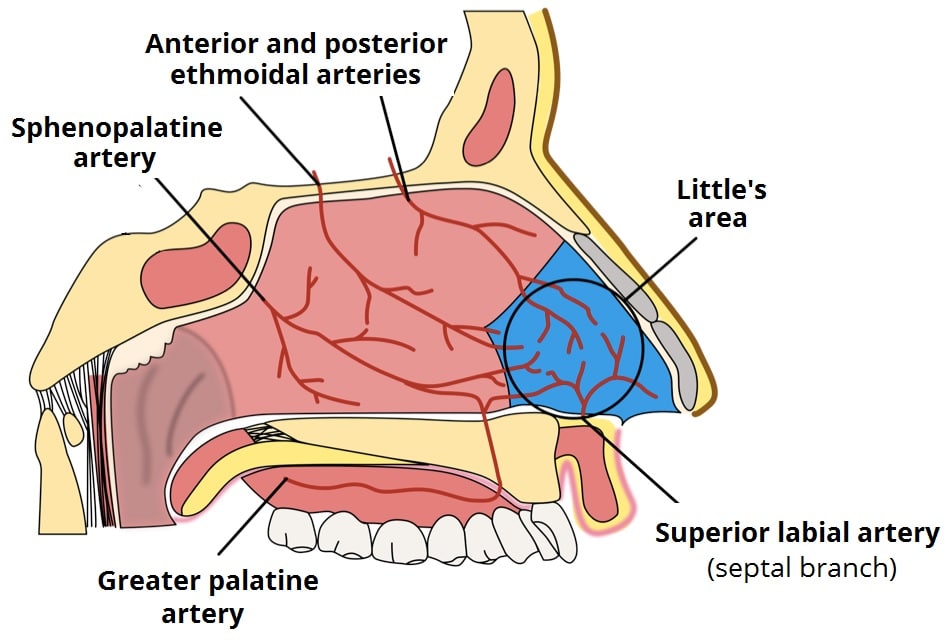
- Anterior bleeds – originate from ruptured blood vessels in Little’s area, a highly-vascularised region formed by the anastomosis of 5 arteries, and cause around 90% of cases
- Posterior bleeds – originate from the posterior nasal cavity, typically from branches of the sphenopalatine arteries of the nose, and cause around 10% of cases (more common in older patients)
Little’s Area
Little’s area (also known as Kiesselbach’s plexus) is found on the anterior nasal septum (Fig. 1) and is an anastomosis of 5 arteries: anterior ethmoidal artery, posterior ethmoidal artery, sphenopalatine artery, greater palatine artery, and the septal branch of the superior labial artery.
There are numerous causes for epistaxis to consider, including trauma, hypertension, iatrogenic (e.g. anti-coagulants), or foreign bodies (nose-picking is the most common cause in children!)
Less common causes include coagulopathies, platelet disorders, vascular malformations, vasculitis, rhinosinusitis (including allergies), malignancy, or cocaine use.
Clinical Features
Enquire about onset, duration, progression, and trigger of the epistaxis, and determine whether likely the initial bleed came through the nose first (anterior bleed) or first noticed bleeding at the back of the throat first (posterior bleed).
As with any nasal condition, it is important to enquire about laterality of symptoms (in this case which side did it bleed from), alongside other nasal symptoms such as nasal obstruction, congestion, discharge and anosmia.
Other symptoms such as facial pain*, otalgia, systemic symptoms should be enquired about, as these suggest a less common or serious cause.
Any recent trauma, co-morbidities or familial conditions (especially clotting abnormalities), relevant drug history (antiplatelets or anticoagulants), and any previous episodes should also be clarified.
*Albeit rare, facial pain or otalgia may indicate a nasopharyngeal tumour (including angiofibroma)
Every case of epistaxis should be initially approached as if severe, until deemed otherwise. Indeed, a patient having a large bleed may be bleeding posteriorly and swallowing a large volume of blood, therefore showing seemingly little external bleeding.
In cases of life-threatening epistaxis (large volume bleeds, haemodynamic compromise, failure to stop post-intervention), an A to E approach to the patient is essential; ensure appropriate airway-trained personnel are present, adequate intravenous access obtained, and resuscitation with blood products if required.
Initial Management
The definitive management of ongoing epistaxis occurs in a stepwise manner, starting with conservative measures. Ensure routine bloods (including FBC, clotting screen, and Group & Save) have been sent and any reversible underlying causes (e.g. malignant hypertension, coagulopathies) managed as required.
All patients (even severe cases) should be kept sat up and sat forward, attempting to ensure blood passes anteriorly and out through the nares (and not posteriorly into the pharynx). Encourage the patient to spit out any blood in their mouth if present.
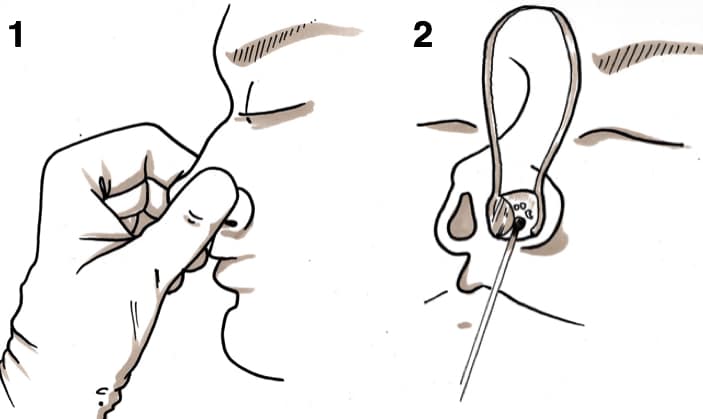
Compression should be applied to the soft lower cartilage portion of the nose (the nares) for 20 minutes without releasing pressure (Fig 2). Ice can be applied to the bridge of the nose to stimulate further vasoconstriction.
If unsuccessful, a Thudicum can be used to inspect the septum. If an anterior bleeding point is identified, the vessel can be cauterised using silver nitrate (Fig. 2).
If there is too much blood present to visualise the septum, adrenaline-soaked cotton wool ball can be inserted into the nasal cavity to cause localised vasoconstriction. Suctioning out excess blood will also help with examination.
Once the bleeding slows, the examiner will have better visualisation of the Little’s area and can cauterise as necessary. Once cauterisation is successful, the patient can be discharged with Naseptin cream or Bactroban ointment to allow the cauterisation area to heal well.
*Avoid cauterising bilaterally at the same time as that increases risk of septal perforation; generally allow 3-4 weeks in between cauterisation either side if there are bilateral bleeding points.
Further Management
If the epistaxis persists but no bleeding point is visualised, anterior packing should be trialled, whereby a nasal pack is inserted into the nasal cavity (Fig. 3) to apply pressure onto the septum to stop the bleed. If this still fails to control the bleeding, then a contralateral nasal pack can also be inserted.
If the epistaxis persists and posterior bleed is suspected, a posterior pack (Rapid Rhino with double balloon) should be inserted. If that fails, the next step would be posterior packing with a Foley catheter, along with BIPP gauze (Fig. 3). As before, if this fails to control the bleeding, then a contralateral pack should be inserted.
Nasal packs should be left in-situ for 24 hours to ensure the bleeding vessel is well coagulated. After 24 hours, the balloon can be deflated and pack removed, with nasal cavity inspected again to see if there is any cauterisation necessary.
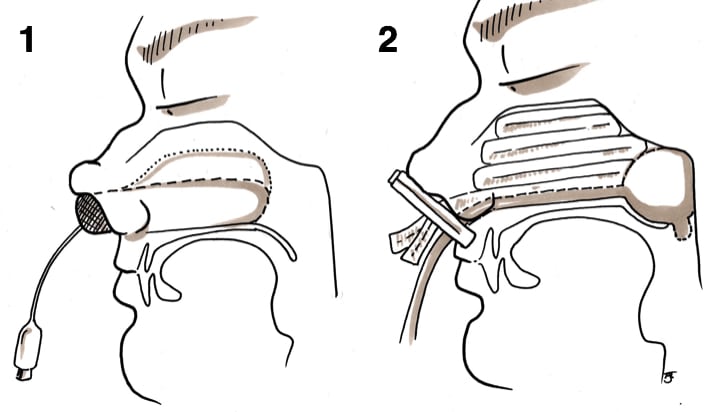
Figure 3 – IIllustrations demonstrating (1) Anterior packing (2) Posterior packing with Foley catheter + BIPP pack
Surgical Intervention
If nasal packing fails to stop the bleeding, then contributing blood vessels can either be ligated surgically or embolised radiologically.
The vessels that are targeted are usually the sphenopalatine artery, anterior ethmoidal artery (never embolised due to its origin from the internal carotid artery and may lead to blindness), or the external carotid artery (as a last resort).
Key Points
- There are numerous causes for epistaxis to consider, including trauma, hypertension, iatrogenic, or foreign bodies
- Anterior bleeds form 90% of all cases of epistaxis, most arising from Little’s area
- A sequential approach is required for all cases of epistaxis management, with conservative approach being the basic management of epistaxis