Introduction
Hydrocephalus is the accumulation of cerebrospinal fluid (CSF) within the cerebral ventricles. From the presence of increased CSF, ventricular dilatation occurs, which can in turn lead to white matter damage, gliotic scarring, and eventual in death if left untreated.
In this article, we will cover the clinical features, investigations and management options of hydrocephalus.
Pathophysiology
Hydrocephalus can also be classified into non-communicating (obstructive) and communicating (non-obstructive):
- Obstructive hydrocephalus is caused by a blockage to the natural ventricular drainage system and CSF flow
- Communicating hydrocephalus is due to reduced absorbance of CSF by the arachnoid villi (or rarely due to increased CSF production)
|
Obstructive |
Communicating |
| Obstructing tumour or cyst
Congenital (e.g. congenital aqueduct stenosis) |
Infective meningitis
Subarachnoid haemorrhage Congenital (e.g. Dandy-Walker syndrome) Normal Pressure Hydrocephalus |
Table 1 – Causes of Hydrocephalus; around one third of cases of hydrocephalus are idiopathic
Normal Pressure Hydrocephalus
Normal pressure hydrocephalus (NPH) describes ventricular dilatation present in the absence of raised CSF pressure. Around 50% of causes are idiopathic, with the remainder due to SAH, meningitis, head injury, or malignancy.
It presents classically with a triad of Parkinsonian gait, urinary incontinence, and dementia. On CT imaging, there will be ventricular enlargement, which is in excess to sulcal atrophy and periventricular lucency. CSF pressures on lumbar puncture will be normal.
The mainstay of treatment is through surgical insertion of a CSF shunt. Most cases, especially if diagnoses and treated early, will obtain a clinical benefit from intervention.
Clinical Features
Patients will present with nausea & vomiting and headache, typically worse in the morning following the long-period of lying supine.
As the condition progresses, there may be altered GCS, blurred vision, gait abnormalities, and incontinence. Papilloedema may also be evident on examination.
Congenital Hydrocephalus
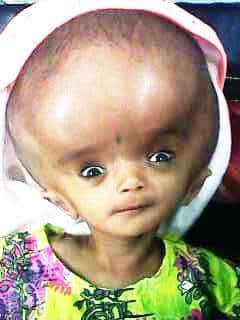
Figure 2 – A infant girl demonstrating sunset sign, prior to shunt insertion
Causes of congenital hydrocephalus include Bickers-Adams syndrome, Dandy-Walker malformation, or Arnold-Chiari malformation
Infants with congenital hydrocephalus will have distinctive clinical features:
- Rapid increase in head circumference, with dilated scalp veins
- Bulging of the fontanelles
- Eyes pointing downwards with the upper lids retracted (termed ‘sunset sign’)
Early management and correction of congenital hydrocephalus can optimise long-term outcomes.
Investigations
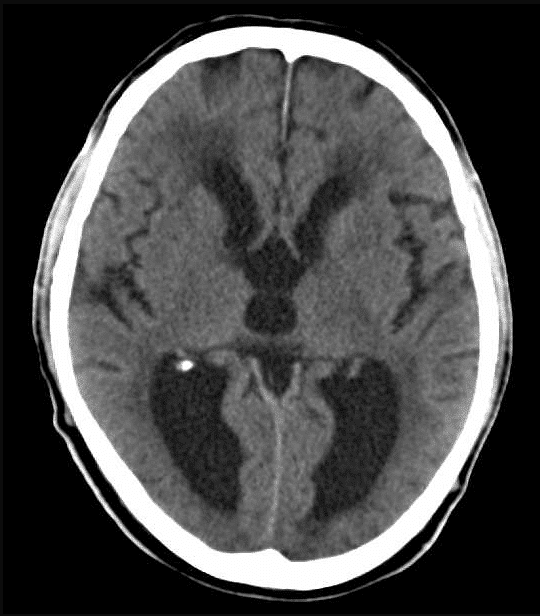
For most cases, CT imaging is the mainstay of initial investigation*, most evidently demonstrating enlargement of the ventricles (however this is not present in every case of hydrocephalus).
Other features of hydrocephalus on CT imaging include loss of the sulcal gyral pattern and CSF exudation from the ventricles (appearing as a subtle hypodensity tracking around the ventricular margins).
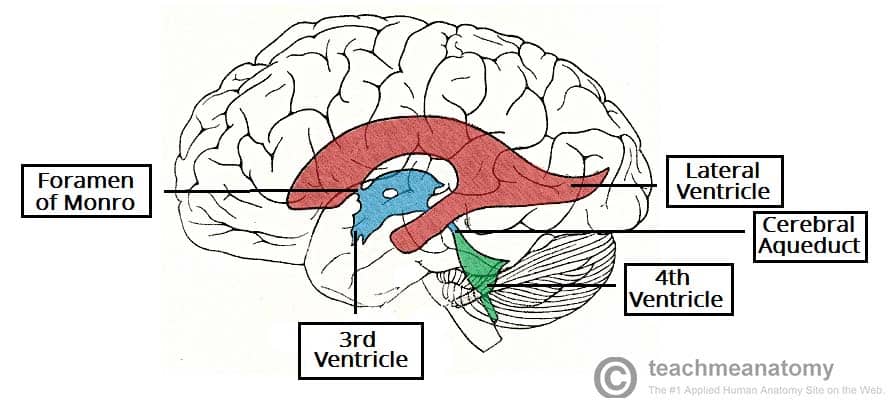
The pattern of ventricular enlargement can help also to determine the underlying cause:
- Generalised ventricular dilatation suggests a communicating hydrocephalus
- Dilated lateral and third ventricle:
- With a normal fourth ventricle suggests aqueduct stenosis
- With dilated fourth ventricle suggests a posterior fossa mass
*Scans through the anterior fontanelles can be used in infants to diagnosis hydrocephalus, avoiding CT imaging
Management
Prompt diagnosis and treatment is key, as delayed treatment increases the risk of damage to brain tissue secondary to the raised intracranial pressure.

Figure 4 – A radiograph demonstrating the positioning of a VP shunt
First-line treatment in the acute setting is usually insertion of an external ventricular drain, acting as a temporary measure to reduce the ICP. Medication* may help to slow progression of the condition, however alone is generally unsuccessful in long-term.
Definitive management will then depend on the underlying cause, for example the debulking of a potentially resectable tumour. Other relieving options include endoscopic third ventriculostomy or choroid plexis resection.
However insertion of a shunt is the most common treatment option used for hydrocephalus. Ventriculo-peritoneal (VP) shunts or ventriculo-atrial (VA) shunts can be inserted as a long-term solution to reduce CSF pressures, reducing CSF fluid and often with their drainage rate controlled through a pressure-sensitive valve.
*Furosemide and acetazolamide act to inhibit secretion of CSF by the choroid plexus, therefore can have a limited role in the management
Key Points
- Hydrocephalus is a build-up of CSF in the ventricular system of the brain, which leads to increased intracranial pressure and potentially fatal consequences
- Diagnosis and effective management of this condition is paramount to reducing the risk of long-term brain injury and death
- The most common form of treatment is a ventricular-peritoneal shunt, but there are other treatment options available