Introduction
A skin abscess is a collection of pus within the subcutaneous tissues, lined by a pyogenic membrane. Skin abscesses are a common clinical presentation, to both primary care and secondary care settings.
A pyogenic skin abscess is different to an infected sebaceous cyst, as whilst both will present with similar clinical features and both contain infected contents, sebaceous cysts are lined with a stratified squamous epithelium
Skin abscess can be classified based on their anatomical location (e.g. perianal abscess or a pilonidal abscess). Patients can also suffer from recurrent abscess formation, which can often be due to an underlying cause, such as perianal fistulae, hidradenitis suppurativa (discussed below), or inflammatory skin conditions.
In this article, we shall look at the risk factors, clinical features, and management of a skin abscess.
Pathophysiology
The main organism involved in skin abscess formation is S. aureus, however multiple skin commensals can cause their formation.
Skin abscess of form when there is a breach to the skin’s defensive barrier, leading to inoculation of pathogens in the subcutaneous tissue.
The resultant acute inflammatory response results in non-specific host tissue damage (Fig. 1), resulting in necrotic tissue and non-viable immune cells forming, termed pus; this becomes surrounded by the pyogenic membrane.
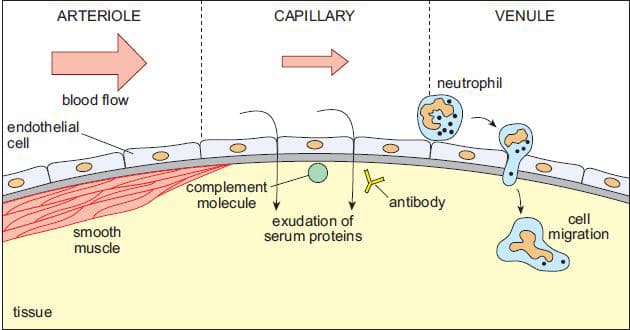
Figure 1 – The stages of acute inflammation, including vessel vasodilation, exudate formation, and neutrophil migration
Panton-Valentine Leucocidin
Panton-Valentine Leucocidin (PVL) is a cytotoxin produced by Staphylococcus Aureus. PVL causes leukocyte and tissue destruction and is produced by <5% of S. aureus strains.
PVL-positive infections are associated with recurrent skin infections and abscess formation, as well as life-threatening infections such as necrotising pneumonia or necrotising fasciitis and osteomyelitis, especially in young previously healthy patients.
Risk Factors
The main risk factors for developing a skin abscess include diabetes mellitus, patients on steroids or any immunosuppressive medication, sickle cell disease, intravenous drug users, or malnutrition.
Clinical Features
Patients with a skin abscess will present with a localised erythematous tender swelling, that may or may not be discharging purulent material (Fig. 1). There may be an associated history of trauma or localised skin condition, results in the initial pathogen inoculation.
On examination, there will be a tender and fluctuant swelling, with surrounding cellulitis. In severe cases, there may be extensive cellulitis and features of sepsis.
Investigations
The majority of skin abscesses can be diagnosed clinically.
In patients with clinical equipoise regarding the diagnosis or in severe cases, routine blood tests, including the full blood count and C-reactive protein, can be performed.
Imaging is rarely required in the investigation of skin abscesses, however it may be warranted if a deeper abscess is suspected yet clinical examination cannot confirm. Depending on the location and subtype, ultrasound scans, CT scan, and MRI scan can all be used to diagnose an abscess formation.
Management
Patients with a skin abscess should be started on empirical antibiotics and adequate analgesia provided. In patients showing clinical features of sepsis, appropriate fluid resuscitation and broad-spectrum antibiotics should be started.
As an abscess does not have a blood supply, antibiotic therapy alone will not resolve all abscesses. The definitive management for any sizeable skin abscess is with an incision and drainage (see video); the specifics of the operation is dependent on the size and location of the abscess.
Incision and drainage allows for drainage of the pus to ensure appropriate source control, reducing the potential overall morbidity and the subsequent risk of recurrence.
If left untreated, the infective process may progress into further cellulitis, necrotising fasciitis, or sepsis.
Hidradenitis Suppurativa
Hidradenitis Suppurativa (HS) is a condition of chronic and recurrent infections affecting the apocrine gland-bearing areas of the body. It is characterised by multiple superficial abscesses, with or without features of chronic sinus formation or ulceration.
Patients present with the condition from adolescent years onwards, affecting 1-2% of the population (with a known genetic predisposition) and is more common in females.
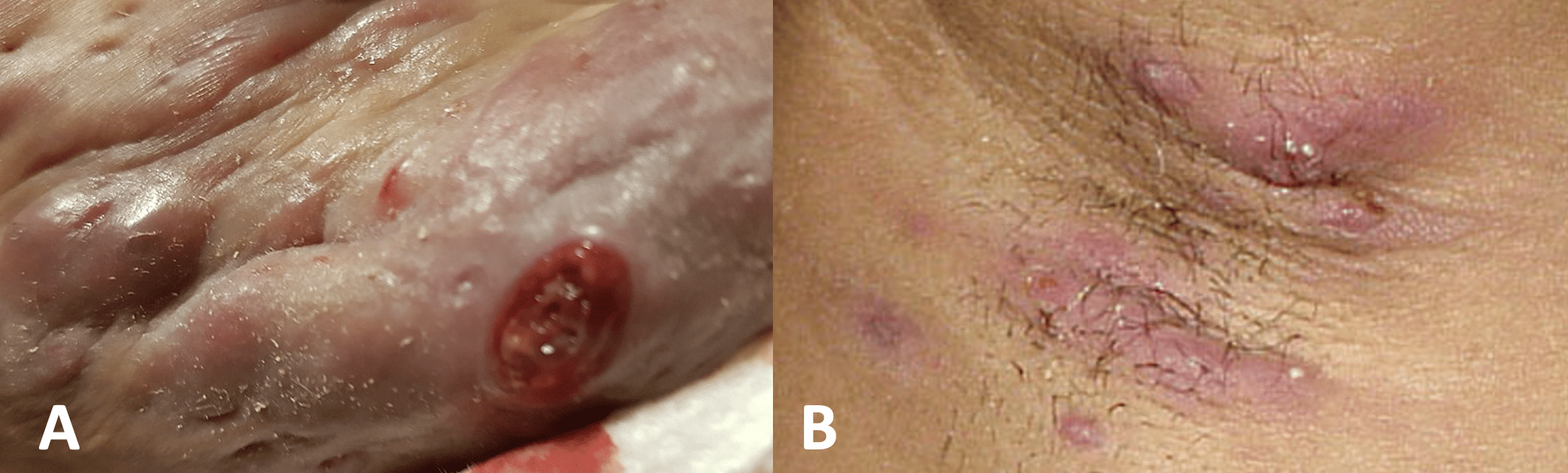
Figure 3 – Hidradenitis Suppurativa (A) Severe (B) Mild
Clinical Features
HS is a diagnosis that is made clinically (Fig. 3). Patients will present with recurrent abscess formation, often resulting in sinus formation due to the breakdown of the apocrine gland walls. There can be eventual surrounding fibrosis of the affected areas due to recurrent infections.
Hurley classification
The severity of HS can be classified using the Hurley classification:
- Type 1 (mild) – isolated lesions with no sinus tracking and minimal scarring
- Type 2 (moderate) – recurrent and multiple abscesses, with features of sinus formation and scarring
- Type 3 (severe) – diffuse disease affecting the majority of a region, with characteristic multiple coalesced abscesses and inflammatory plaques
Management
Management depends on the severity of the disease. Alongside pharmacological and surgical options, ensuring appropriate patient education, smoking cessation, and weight management services are offered where applicable.
Initial management involves use of topical agents, such as Clindamycin solution and Chlorhexidine wash. Long-term oral antibiotics can further be trialled, such as oral tetracycline in milder disease or oral clindamycin with rifampicin more severe disease.
If there is a lack of response to the above treatment, then subsequent treatment options include retinoids (e.g. Acitretin), antimicrobials (e.g. Dapsone) or immunotherapy (e.g. Adalimumab or infliximab), yet these will only be started in secondary care by dermatology teams.
Referred to plastic surgeons should be considered if medical managements fail, which would involve surgical excision of the region, with potential need for future reconstruction with skin grafts or flaps.
Key Points
- A skin abscess is a collection of pus within the subcutaneous tissues, lined by a pyogenic membrane
- Diagnosis is mainly clinical
- Definitive management is with an incision and drainage
- Hidradenitis Suppurativa is a condition of chronic and recurrent infections affecting the apocrine gland-bearing areas of the body

