This article is for educational purposes only. It should not be used as a template for consenting patients. The person obtaining consent should have clear knowledge of the procedure and the potential risks and complications. Always refer to your local or national guidelines, and the applicable and appropriate law in your jurisdiction governing patient consent.
Overview of Procedure
There are several types of hernia, the most common being inguinal, femoral, and umbilical. Repairs can be done both open or laparoscopically, especially for inguinal hernia. The mesh used during the repair is secure in place using tacks.
Laparoscopic procedures have been shown to reduce post-operative pain and allow for faster recovery and return to work. For inguinal cases, laparoscopic repair may also be favoured in patients with bilateral or recurrent inguinal hernia.
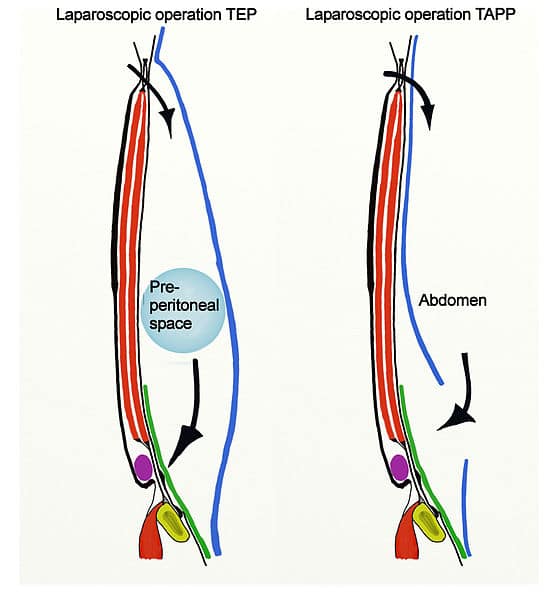
The two commonly employed techniques for laparoscopic inguinal hernia repair are TEP (Totally ExtraPeritoneal) and TAPP (TransAbdominal PrePeritoneal), depending on the layers involved and opened during the repair (Fig. 1).
Complications
Intraoperative
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Haemorrhage | Injury can occur to inferior epigastric vessels (especially with a TEP repair) or external iliac/ femoral vessels | Ensure careful deployment of tacks when securing the mesh |
| Injury to surrounding structures including bowel, bladder and ureter, liver, spermatic cord | Contents of the hernial sac may include these structures | |
| Bowel resection | Incarcerated hernias may contain ischaemic bowel; if the bowel is not viable it must be resected. | |
| Conversion to open | In some cases anatomy may be difficult and it is safer to proceed to an open anterior inguinal hernia repair.
In TEP repairs the peritoneum may be breached and the decision made to convert to TAPP repair. |
|
| Anaesthetic Risks | Includes damage to the teeth, throat and larynx, reaction to medications, nausea and vomiting, cardiovascular and respiratory complications | Forms a part of the anaesthetist assessment before the operation |
Early
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Pain | Use of laparoscopic surgery, compared to open surgery, will limit post-operative pain | |
| Bleeding/ haematoma | There is a small chance of bleeding and bruising in the abdomen post-surgery | Haematoma or seroma formation are usually self-limited due to the tamponade of the peritoneum |
| Infection | Superficial wound infection is possible. An infected mesh is a fortunately rare but serious complication, as would be revision of wound | Peri-operative antibiotics will reduce the risk of wound infections |
| Scarring | Laparoscopic surgery will minimise this risk | |
| Altered sensation | Damage to ilioinguinal and/or genitofemoral nerve | |
| Seroma | A swelling of lymphatic fluid may occur in redundant subcutaneous space following surgery | |
| Testicular Atrophy | Damage to the blood supply to the testicle can occur in groin hernia repair, often due to venous thrombosis rather than arterial injury | Identify and avoid damage to the spermatic cord and associated vessels |
| Scrotal swelling/ hydrocoele | Damage to venous/ lymphatic drainage during dissection | |
| Blood Clots | The patient will be given anti-embolism stockings and low molecular weight heparin peri-operatively to minimise this risk as deemed appropriate | |
| Stroke, MI, Kidney Failure, Death | Although small, this is always a risk in any major surgery |
Late
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Adhesions | Abdominal surgery may cause adhesions as a reaction to the procedure, although this is uncommon (especially in TEP repair) | |
| Recurrence | There is always a potential for further surgery due to recurrence of the hernia. For inguinal hernia it is around 1% at 5 years. | Request the patient avoids strenuous activity for a few weeks post-operatively |