Introduction
Cystic neoplasms of the pancreas are a group of pancreatic lesions defined by the presence of an epithelial-lined wall and typically fluid-filled (or less commonly rich in mucin or a solid component).
The vast majority are benign and are found incidentally, however some have potential for malignant transformation and therefore appropriate investigation is indicated to determine the need for surgical removal or long-term surveillance.
Pancreatic cysts are largely asymptomatic, however due to the increased use of cross-sectional imaging in recent years, their incidence is increasing. Current estimates place the prevalence of pancreatic cysts in the general population at around 8%.
Pancreatic cysts are different to pseudocysts, which are fluid-filled regions that occur anywhere within or adjacent to the pancreas, however lack an epithelial-lined wall and are generally a long-term sequela to pancreatitis.
Clinical Features
Pancreatic cystic lesions are generally identified incidentally on imaging, but may present with space-occupying features, such as abdominal pain, distension, gastric outlet obstruction, jaundice, acute pancreatitis, or weight loss secondary to exocrine insufficiency.
Given their incidental nature, examination is generally unremarkable, although large cysts may be palpable on abdominal examination. In the presence of biliary obstruction, clinical jaundice may be evident.
Investigations
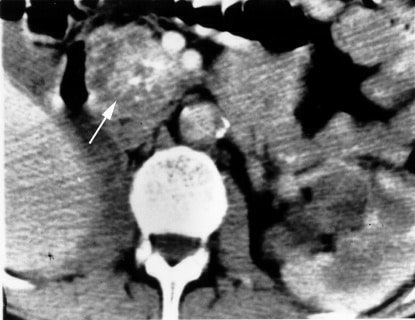
Cystic lesions of the pancreas should be characterised by a combination of ultrasound, CT imaging, and MRI imaging, often in conjunction with endoscopic ultrasound (EUS), often used in sampling of cyst fluid by fine needle aspiration (FNA) and biopsy. This allows for the definition of the subtype of the lesion, to exclude malignancy (and enable estimating of malignancy risk).
Radiological characteristics often allow for diagnosis of cyst subtype, but where further analysis is required, EUS with FNA is indicated which allows cytological examination and biochemical analysis of cyst fluid for Ca19-9, Ca125, amylase, and CEA (Table 1)
Cyst Subtypes
Cysts may be defined by their content as serous or mucinous, with the most commonly encountered cystic neoplasms in the pancreas being serous cystadenoma (SCA) (30-40%), mucinous cystic neoplasm (MCN) (10-45%) and intra-ductal papillary mucinous neoplasm (IPMN) (20-30%), with rarer types including solid pseudopapillary neoplasm (<10%) and cystic endocrine neoplasm (<10%).
For each cystic lesion subtype, a number of features have been identified which increase the risk of malignant transformation. Presence of these features should lead to closer surveillance or assessment for surgical resection.
- SCA have a low malignant potential of around 3%, but tumours over 40mm, those with rapid growth, or those causing symptoms may warrant resection
- MCN high risk features include those sized >40mm or any enhancing mural nodule on imaging
- IPMN high risk features include the presence of jaundice, any enhancing mural nodule ≥5mm on imaging, or the main pancreatic duct ≥10mm
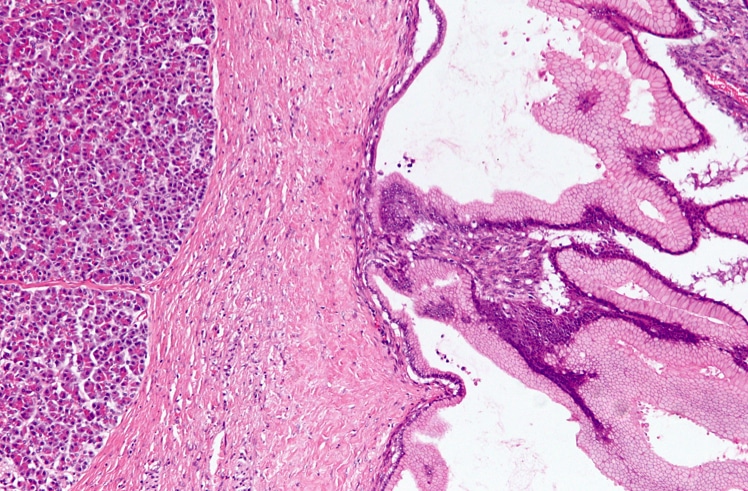
| Cyst Type | Radiological Features | Fluid Appearance | Biochemical Features | Cytological Features |
| Serous cystadenoma | Multiple cysts within single lesion with central scar | Thin +/- blood staining | Amylase – Low
Ca19-9 – Variable CEA – Low Ca125 – Low |
Cuboidal cells with clear, glycogen-rich cytoplasm |
| Mucinous cystic neoplasm | Single cystic lesion +/- small number of septations | Mucinous | Amylase – Low
Ca19-9 – Variable CEA – High Ca125 – Variable |
Columnar mucinous cells with variable atypia |
| Intra-ductal papillary mucinous neoplasm | Mixed with possible pancreatic duct dilation | Mucinous | Amylase – High
Ca19-9 – Variable CEA – High Ca125 – Low |
Columnar mucinous cells with variable atypia |
Table 1 – Features defining common pancreatic cystic neoplasms on radiological and endoscopic ultrasound assessment (adapted from Brugge WR et al)
Management
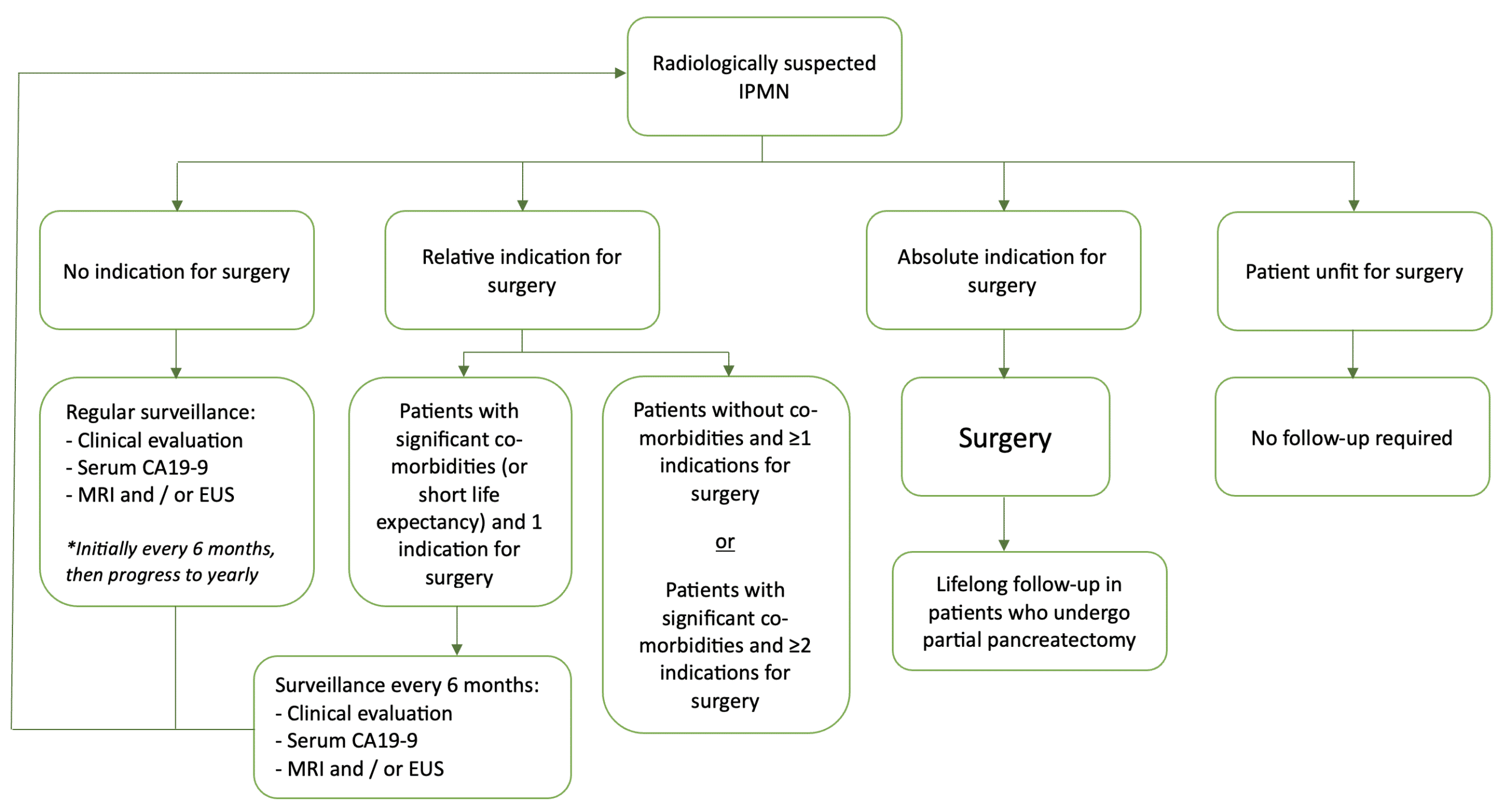
Newly diagnosed pancreatic cystic neoplasms should be referred to specialist HPB multidisciplinary team (MDT) meeting for discussion and appropriate follow-up.
Symptomatic cysts and cysts with high-risk features should be considered for surgical resection. For IPMN specifically, indications for surgery include:
- Absolute indications for surgery – positive cytology for malignancy or high grade dysplasia, solid mass, presence of jaundice (due to the tumour), enhancing mural nodules >5mm, or main pancreatic duct ≥10mm
- Relative indications for surgery – growth rate >5mm/year, increased CA19-9 serum levels, main pancreatic duct 5 – 9.9mm, cyst diameter >40mm, enhancing mural nodules <5mm, new-onset diabetes mellitus, or acute pancreatitis (from IPMN)
Patients IPMN or MCN who are surgical candidates but without high-risk features are recommended to undergo surveillance. MRI pancreas as the recommended surveillance imaging modality (Fig. 4). Should a patient not be a surgical candidate or not wish for surgical intervention, surveillance can be discontinued.
Prognosis
The prognosis of these patients is highly dependent on subtype of the cyst; non-malignant and non-invasive cysts will have excellent prognosis, whilst those which harbour malignancy have a prognosis similar to early stage pancreatic adenocarcinoma
Key Points
- Pancreatic cysts are fluid-filled lesions found within the pancreas, usually asymptomatic
- Most pancreatic cysts are found incidentally and require formal characterisation with CT pancreas or MRCP imaging and endoscpic ultrasound
- A combination of history, examination, radiological features, fluid cytology, and biomarker analysis frequently can diagnose the type of pancreatic cyst and determine the risk of malignant transformation
- Symptomatic cysts, cysts with high-risk features, and those with known high risk for malignancy should be referred for surgical resection, the remainder can undergo regular surveillance