Introduction
Elbow dislocations usually occur in older children and young adults (between 10 – 20yrs) and account for up to 25% of elbow injuries.
An elbow dislocation is defined as simple or complex*, the latter being associated with a concomitant fracture. 90% of elbow dislocations occur posteriorly, with 50% suffering bony injury.
The elbow’s stabilising elements are damaged during traumatic dislocation and loss of all static stabilisation (primary and secondary) will lead to ongoing instability.
*Elbow dislocations are less common in young children; a supracondylar fracture of the distal humerus should be suspected when a child has a deformed and painful elbow
Elbow Joint Stability
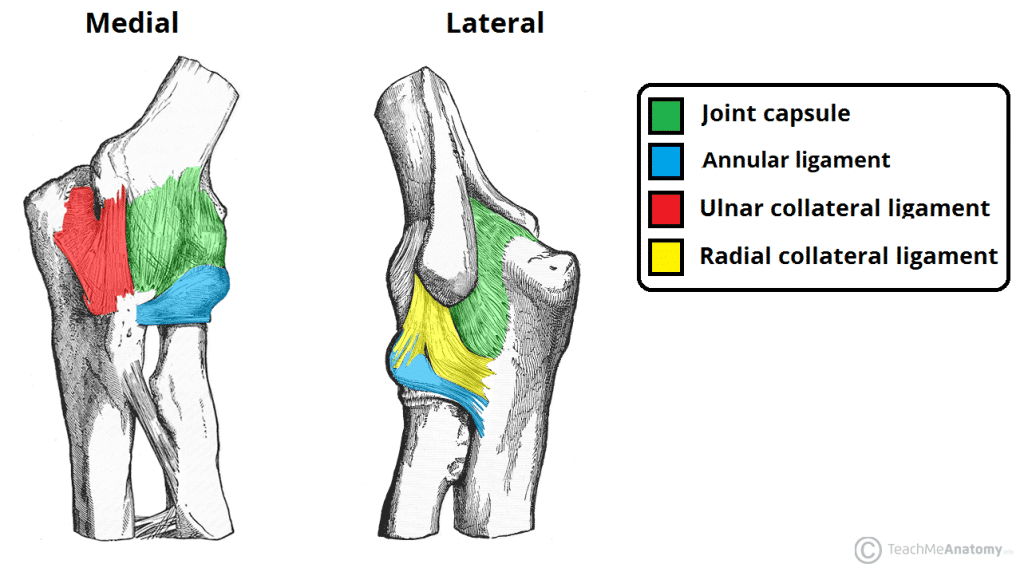
The elbow joint is stabilised by static and dynamic stabilisers.
The humeroulnar joint and the medial and collateral ligaments make up the primary static stabilisers, whilst the radiocapitellar joint, joint capsule, and the common flexor and extensor origin tendons make up the secondary static stabilisers.
Dynamic stabilisers consist of the surrounding musculature of the elbow joint, with the anconeus, brachialis, and triceps brachii all contributing to this variable stability.
Clinical Features
Patients typically present following a high-energy fall.
The joint will be painful and deformed, with associated swelling and decreased function (usually near immobile in near full extension with disruption of the equilateral triangle of the elbow)
A complete neurovascular examination of the upper limb is essential:
- A deficit is often found in the territory of the ulnar nerve as neuropraxia of this nerve is common
- A good capillary refill can be found even in those with an arterial injury, due to the elbow having a rich collateral circulation
Investigations
Any patients presenting with significant trauma should be resuscitated, investigated, and managed as per ATLS protocols.
For otherwise stable patients, plain film radiographs of the elbow, both AP and lateral, are required initially. Elbow dislocations can be identified from the loss of the radiocapitellar and ulnotrochlea congruence (the anterior humeral line and radiocapitellar line will aid in assessing this).
CT imaging is only really useful as an adjunct in cases with associated fractures.
Management
Initial management, following examination and documentation of neurovascular status, requires closed reduction (see below).
Ensure sufficient analgesia +/- sedation if appropriate, and apply an above elbow backslab once reduced to keep the elbow at 90 degrees.
Further management post-reduction is dependent on the presence of an associated fracture. The extent of soft tissue damage will dictate the stable position; if the lateral collateral ligament is damaged the elbow will be more stable in pronation, if the medial collateral ligament is disrupted the elbow will be more stable in supination.
For a simple elbow dislocation with no fracture, further orthopaedic management can be as an outpatient, following with a short period of immobilisation (5-14 days, depending on local practice). Early rehabilitation with supervised range of motion exercises in the stable arc can be introduced.
If the dislocation is complicated by a fracture, open type injury, or has neurovascular compromise, then operative fixation can be considered. This involved open reduction and internal fixation (ORIF) of the coronoid, radial head, or olecranon with appropriate soft tissue repair (LCL and MCL).
Closed Reduction of an Elbow Dislocation
Two basic methods are possible for closed reduction of an elbow dislocation, either via in line traction method or via manipulation of the olecranon (in a distal and anterior direction).
Following this, the elbow can be flexed to 90 degrees to reassess the equilateral triangle of the elbow, which should now be restored. Apply an above elbow back slab to keep the elbow at 90 degrees.
A plain film radiograph is needed to confirm reduction. Neurovascular status should be carefully re-assessed and documented.
Complications
A common complication of elbow dislocation is early stiffness with loss of terminal extension, however early treatment and rehabilitation reduce this risk.
The most common neurovascular injury is stretching of the ulnar nerve. Fortunately, injury to the brachial artery and associated median nerve is rare.
Recurrent instability can be an issue with some patients and such cases would warrant a discussion regarding future surgery. However, adequately treated simple dislocations have a low recurrence rate of <2%.
Terrible triad
The Terrible Triad injury refers to an elbow dislocation with (1) lateral collateral ligament injury (2) radial head fracture (3) coronoid fracture
This combination of injuries causes a very unstable elbow and is associated with a poor outcome. The forces applied to the joint result from a fall onto an extended arm with rotation, resulting in a posterolateral dislocation. Patients are likely to have recurrent problems with instability, stiffness, and arthrosis.
Treatment revolves around operative fixation of each of the components. Radial head ORIF or arthroplasty with LCL reconstruction and coronoid ORIF and MCL reconstruction is also sometimes undertaken following intra-operative assessment.
Key Points
- Elbow dislocations can be classified as simple or complex, depending on associated fractures
- Patients typically present following a high-energy fall, with a painful and deformed joint
- Assessment of neurovascular status of the limb throughout management is essential
- Post-reduction, further management depends on whether simple or complex dislocation
- The “Terrible Triad” injury refers to an elbow dislocation with (1) lateral collateral ligament injury (2) radial head fracture (3) coronoid fracture