Introduction
The most common site of shoulder fracture is the proximal humerus, accounting for around 5% of all fractures.
The majority of proximal humeral fractures are low energy injuries occurring in elderly patients falling onto an outstretched hand from standing. These injuries occur primarily in the context of an osteoporosis.
They also less commonly occur in younger patients usually the result of a high energy traumatic injury, therefore there are often associated soft tissue or neurovascular injuries.
Risk Factors
The risk factors for low energy proximal humerus fractures are comparable to other osteoporotic fractures, including female gender, early menopause, prolonged steroid use, recurrent falls, and frailty.
Clinical Features
The principal features of this injury will be pain around the upper arm and shoulder, with restriction of arm movement and an inability to abduct their arm.
On examination, there is likely to be significant swelling and bruising of the shoulder, which can spread to the chest and down the arm.
Due to the close anatomical relationship with the axillary nerve and the circumflex vessels, is important to check the neurovascular status of the arm; damage to the axillary nerve can result in loss of sensation in the lateral shoulder (“Regimental Badge Area”) and loss of power of the deltoid muscle.
Investigations
As for any trauma case, urgent bloods, including a coagulation and Group and Save, should be sent. Where a pathological cause is suspected, further work-up bloods, such as a serum calcium and a myeloma screen, may be warranted.
Plain film radiographs are the required initial imaging modality for suspected shoulder fracture. To appropriately to visualise and classify a proximal humeral fracture, anteroposterior (AP), lateral scapular, and axillary views are all required.
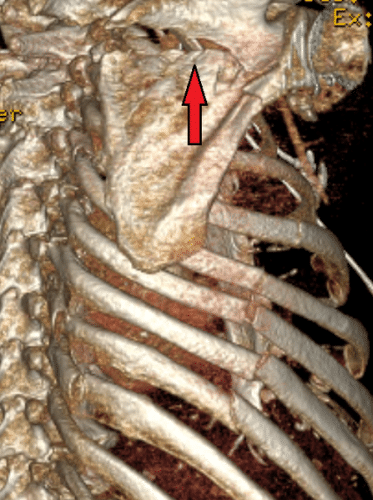
Further imaging with a CT scan can be used for preoperative planning, or if the position of any of the humeral segments is unclear.
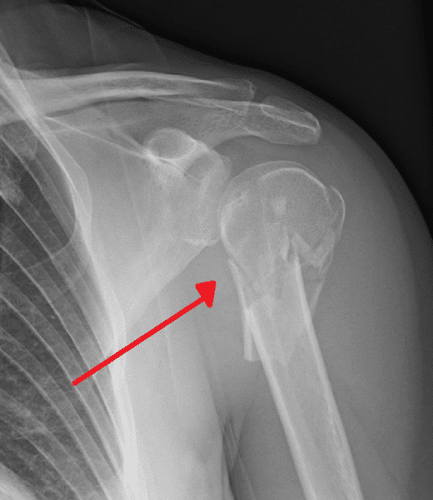
Figure 2 – A comminuted proximal humeral fracture
Classification
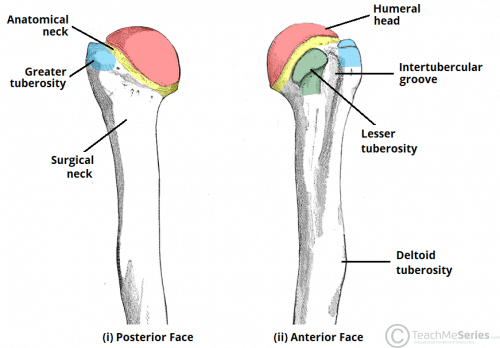
The Neer classification system* is used to characterise proximal humeral fractures based on the relationship between 4 main segments of the proximal humerus:
- Greater tuberosity
- Lesser tuberosity
- Articular segment (anatomical neck)
- Humeral shaft (surgical neck)
*These segments are considered separate if there is displacement >1cm between segments, or if there is at least 45 degrees of angulation; it categorises injuries into either minimal displacement or two to four part injuries, dependent on the number of separate segments present.
Management
The majority of proximal humeral fractures can be managed conservatively, especially those minimally displaced without neurovascular compromise.
The patient requires immobilisation initially with early mobilisation including pendular exercises at 2-4 weeks post injury dependent on fracture pattern. The patient must have a correctly applied polysling that allows their arm to hang; the effect of gravity on the arm will aid the reduction of the fragments of most humeral fractures.
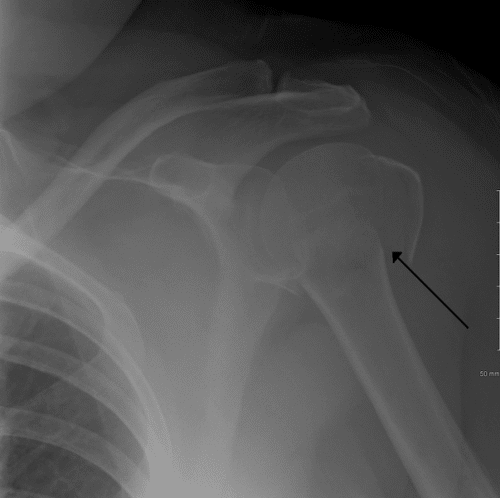
Figure 3 – A proximal humeral fracture across the surgical neck
Surgical Management
Surgical fixation is indicated in patients with displaced, open, or neurovascularly compromised fractures, however the type of surgery is dependent on the classification and complexity of the fracture, and patient factors.
Patients with multiple segment injuries may be managed with open reduction internal fixation (ORIF) or intermedullary nailing. ORIF is often preferred in a head splitting fracture, and intramedullary nailing is preferred if the fracture involves the surgical neck, or if the fracture is combined with a humeral shaft fracture.
Hemiarthroplasty can be performed in a small number patients who experience complex injuries, or injuries that include splitting of the humeral head and are likely to have significant complications if the fracture is treated using ORIF.
Reverse shoulder arthroplasty (RSA) is an option for low demand patients, or patients who require revision after a failed previous procedure. RSA involves a total shoulder arthroplasty in which the ball and socket portions of the shoulder joint are reversed. Usually conservative management will be attempted before arthroplasty.
Complications
The most common complication of a proximal humeral fracture is a reduced range of motion, and extensive physiotherapy will be required to regain full function and reduce pain. Rehabilitation time for a proximal humeral fracture is around 1 year and is very dependent on how soon the patient was allowed to mobilise their shoulder.
There is a risk of avascular necrosis of the humeral head following an injury disrupting the blood supply (from the anterior and posterior humeral circumflex arteries). In such cases, a hemiarthroplasty or reverse shoulder arthroplasty may be required.
Damage to the neurovascular supply is thankfully rare, however it remains essential to check the axillary nerve in these injuries.
Key Points
- The most common site of shoulder fracture is the proximal humerus
- Patients present with shoulder pain and a reduced range of movement, typically following a fall onto an outstretched hand
- The Neer classification system is used to characterise proximal humeral fractures
- Most cases require plain film radiographs only and can be managed conservatively
Scapular Fractures
A scapular fracture is a very rare type of fracture, due to its protection afforded by its surrounding muscles. Scapular fractures are associated almost exclusively with high energy trauma and as a result, patients with scapular fractures have an associated mortality rate of 2-5% due to their concurrent severe injuries.
The vast majority of scapular fractures are treated non-operatively, as up to 90% of fractures are aligned acceptably. Open reduction internal fixation (ORIF) is indicated for individuals with glenohumeral instability, displaced scapular neck, or complex fracture patterns. A floating shoulder results when a scapular neck fracture is associated with a clavicle fracture. This almost always requires fixation.
Patients can expect good results with no functional deficits after nearly all nonoperative cases and in 70% of surgical cases.