Introduction
Ear trauma is common and frequently co-exists alongside other traumatic injuries. All patients with head injuries or trauma should be approached in a structured A to E format.
Injuries that initially appear simple can be complex and could require involvement from multiple inpatient team specialities. Fortunately, most ear trauma does not require urgent management (and the management of any intracranial pathologies will nearly always take priority).
Once the patient is stabilised, any patient with suspected ear trauma should have a full oto-neurological examination performed (see here), including of the cranial nerves. If indicated, as per the NICE guidelines, a CT scan may be required for further assessment*.
In this article, we discuss specific examples of ear-related trauma, including their pathophysiology and management.
*If specifically looking for a temporal bone fracture, fine-slice CT imaging of the temporal bones is advised
Pinna Haematoma
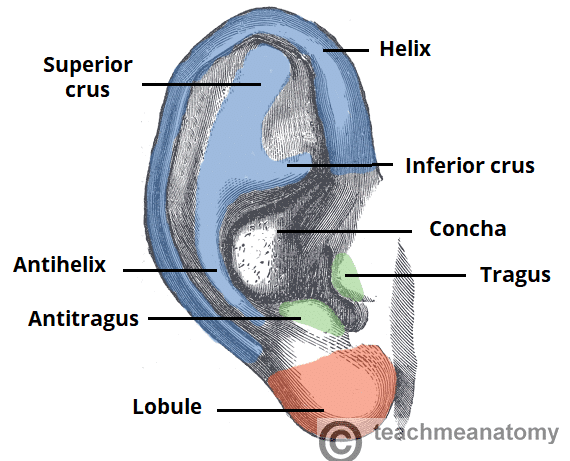
A pinna haematoma is a common injury* that occurs from shearing forces applied to the auricle, most commonly seen amongst rugby players and boxers.
Following initial trauma, the perichondrial blood vessels tear, resulting in haematoma forming between the auricular cartilage and the overlying perichondrium (Fig. 2). Consequently, the blood supply to the underlying cartilage from the perichondrium can become impaired.
If a pinna haematoma is left untreated, then due to the disrupted blood supply, avascular necrosis of the pinna can occur. Subsequent fibrocartilage overgrowth can lead to a structural deformity of the auricle, colloquially termed “cauliflower ear”
*The main differential diagnosis is an auricular pseudocyst, which can develop spontaneously or as a result of trauma; in such cases, serous fluid collects, giving a similar appearance to pinna haematoma
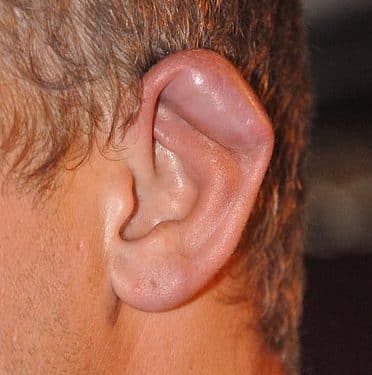
Figure 2 – A patient with an auricular haematoma
Principles of management for auricular haematoma include draining of the haematoma, and pressure dressing after to prevent re-accumulation of haematoma. Due to risk of avascular necrosis, drainage of the haematoma should be performed within 24 hours of the injury.
After evacuation of a haematoma, gauze padding should be placed over the ear and a tight headband applied. If the haematoma re-accumulates, it will require re-drainage. These patients should be reviewed again in a week to remove the pressure dressing, and to ensure that repeat drainage can be done if there is any re-accumulation.
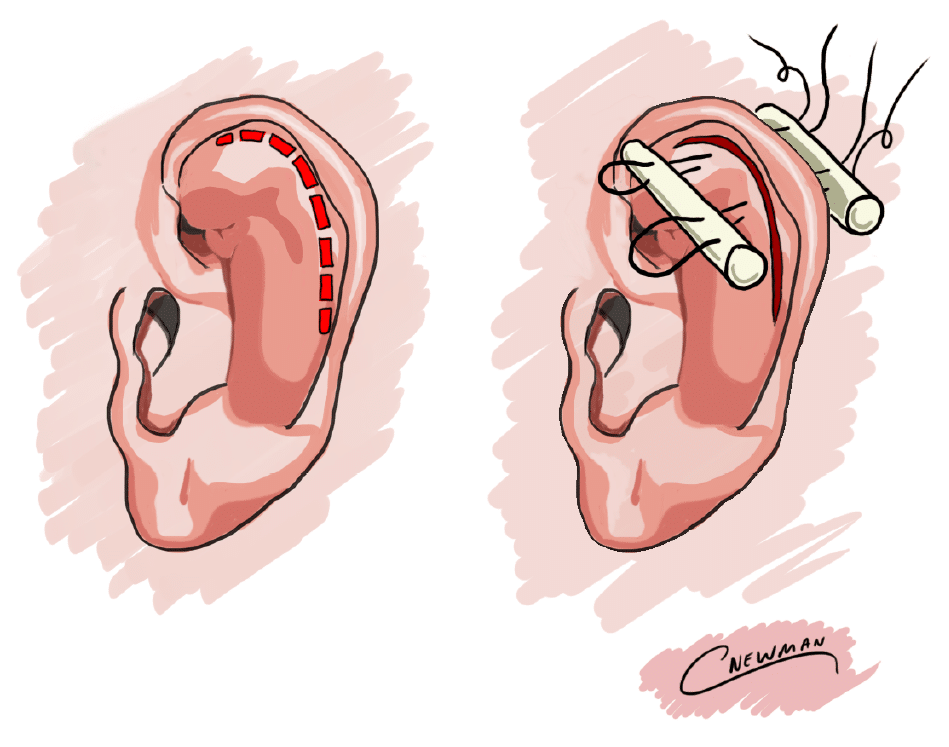
Drainage of a Pinna Haematoma
Ensure an appropriate aseptic field is prepared (ideally in an operating theatre) and instill local anaesthetic (not containing adrenaline) to provide a regional block of the pinna.
An incision along the inside of the helical rim (the point where most fluctuant and least aesthetic compromise) should be made, allowing for the evacuation of the haematoma*. If required, the cavity can be washed out with saline (mixed with iodene if needed).
There are mutliple additional methods to prevent re-accumulation of the haemaotoma; a common technique involves placing a dental roll either side of the auricle and secure these in place using tight mattress sutures around the rolls and through the pinna (Fig. 3). This will apply pressure onto the perichondrial space, aiming to prevent the re-accumulation of blood and restoring cartilage perfusion.
*In small haematomas presenting early, one can consider simple needle aspiration, although this can carry an increased risk of incomplete haematoma evacuation
Pinna Laceration
Pinna lacerations can vary significantly in their severity, however general principles can be considered for their management. To ensure optimal wound healing, ensure thorough wound cleaning under local anaesthetic; consider tetanus boosters and antibiotic prophylaxis if required.
All auricular cartilage should be covered by skin; as the cartilage derives its blood supply from the overlying perichondrium, cutaneous coverage is paramount to prevent avascular necrosis of the cartilage and a good recovery (this can include excising cartilage to achieve this).
Temporal Bone Fracture
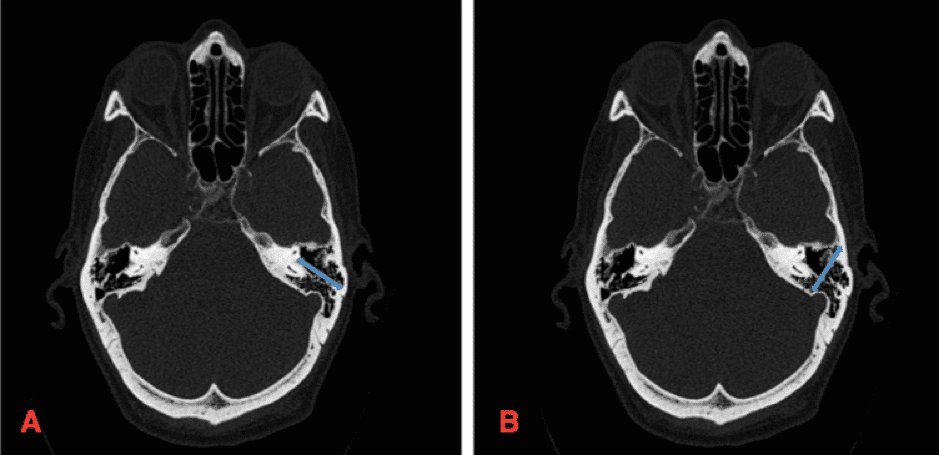
Patients presenting with a head injury and suspected temporal bone fracture need prompt investigation and management. CT imaging of the temporal bones provides the initial mainstay of investigation (Figure 4). However, to have sustained a temporal bone fracture, the patient must have had a relatively high impact injury, therefore ATLS principles with an A to E assessment is essential for all such patients.
Temporal bone fractures can be categorised* as either longitudinal or transverse (many are mixed), depending on their relation to the axis of the ear canal:
- Longitudinal temporal bone fractures are the more common type (~80%), typically occurring from a lateral blow to the head and are usually associated with conductive hearing loss
- Transverse temporal bone fractures occur from fronto-occipital head trauma and are usually associated with sensorineural hearing loss or facial nerve injury
*A more clinically useful categorisation would be classification relating to otic capsule involvement; involvement of the otic capsule carries an increased risk of permanent sensorineural hearing loss, facial nerve palsy, and CSF leak
Clinical signs suggesting a temporal bone fracture should be assessed for, perhaps the most important of which is facial nerve injury. Importantly, any facial nerve palsy immediately after injury is likely as a result of direct damage to the nerve and has a low chance of recovery (delayed onset facial nerve palsy post-trauma is more likely to represent a neuropraxia, secondary to tissue oedema).
Other signs of temporal bone fracture include:
- Post-auricular ecchymosis (termed “Battle’s sign”), usually resulting from rupture of the posterior auricular artery secondary to the basal skull fracture
- Haemotymanum, or other otoscopy signs, including an irregular step in the canal, canal laceration, or tympanic membrane perforation
- CSF otorrhoea or rhinnorhoea (further discussed here)
- Hearing loss, either conductive or sensori-neural, and will typically be multifactorial, however fortunately most cases resolve spontaneously*
All temporal bone fractures should be admitted for neuro-observation. Cases should be discussed by the multi-disciplinary team for consideration of surgical intervention. In practice, the majority of these injuries are managed conservatively.
If there are any concerns of hearing loss these patients are booked for audiology investigations a week later, once swelling and blood in the ear canal subsides.
*Persistent hearing loss may suggest include ossicular chain disruption or tympanic membrane perforation and will need further work-up
Tympanic Membrane Perforation
Tympanic membrane perforation can occur as a result of blunt trauma, penetrating trauma, or barotrauma (albeit most cases overall are infective or iatrogenic). The facial nerve function should be assessed and documented, along with bedside tuning fork hearing tests (Weber and Rinne)
The size and location of the perforation will be seen on otoscopy (Fig. 5). If there is blood in the canal, this may need to be suctioned in order to achieve a good view of the tympanic membrane; substantial volumes of blood in the canal/middle ear may indicate a more complicated injury.
Uncomplicated traumatic perforations of the ear drum will likely heal spontaneously after 2-3 months. Simple perforations do not warrant the use of prophylactic antibiotics, but the patient must be advised on strict ear water precautions in order to reduce the incidence of a secondary infection. Non-healing perforations may require surgical repair (commonly a myringoplasty).

Figure 5 – A Left Tympanic Membrane Traumatic Perforation, as seen on Otoscopy
Key Points
- Immediate assessment and management of all head injuries should be done according to ATLS principles
- Always suspect a more extensive injury than what is immediately visible when assessing a patient with potential otological injury
- Pinna haematoma, temporal bone fracture, and tympanic membrane perforation are all potentially serious conditions associated with ear trauma