Introduction
In appropriate patients, heart transplantation is the final treatment option in end-stage heart failure.
The demand for donor hearts from deceased donors still outweighs the supply, however the number of heart transplants performed has slowly increased in a few high-income countries in recent years. In the UK, there are approximately 200 heart or heart and lung transplants a year.
Patients awaiting their transplants are managed using bridges to transplantation devices, such as ventricular assist devices (VAD) and extracorporeal membrane oxygenation (ECMO).
Indications
Heart transplantation is indicated in patients with end-stage heart failure, which can be secondary to ischaemic heart disease, valvular heart disease, cardiomyopathy (dilated, restrictive, or ischaemic), or congenital heart disease.
Several criteria must be met for patients to be deemed suitable for a donor heart*. Most importantly, patients must be deemed to have refractory disease, such as severe heart failure persisting despite maximal medical treatment or severe coronary artery disease not amenable to interventional or surgical revascularisation.
Contraindications for heart transplantation include irreversible pulmonary hypertension, active systemic infection (such a tuberculosis) or active malignancy, or high BMI (>35)
Risk factors to be considered for worse outcomes of heart transplantation include advancing age (over the age of 60yrs), previous cardiac surgery, ex-smoker, and frailty.
*They should also have a good VO2 max and an estimated 1yr survival >80%
Surgical Techniques
Donor hearts come exclusively from deceased donors. The prospective donors are matched using blood group, HLA status, and heart size.
Donor hearts come exclusively from deceased donors, with the prospective donors matched using blood group, HLA status, and heart size. Heart transplants can occur alone or (rarely) as a combined procedure with a heart and lung transplantation
Donor Procedure
Donor hearts are normally retrieved via a median sternotomy approach. After sternotomy, the heart and lungs are inspected and their function is tested. If abdominal organs are also being retrieved, a laparotomy is also performed to allow for the relevant abdominal viscera to be inspected*.
The donor is infused with heparin systemically and the vena cava are divided, first the superior vena cava and then the inferior vena cava, emptying the right side of the heart. The pulmonary vein is divided, which empties the left side of the heart. At this point a cross-clamp is applied to the distal part of the ascending aorta, above the site for aortic cannulation.
Cold cardioplegia solution is administered and the donor heart is arrested, and ice is applied to the heart to minimise metabolic activity. If the lungs are being retrieved simultaneously, the left atrium is divided to provide adequate tissue for implantation with the lungs. The ascending aorta is then divided just before the brachiocephalic artery and then pulmonary artery is divided at the point of bifurcation, which then frees the heart.
Once the heart is dissected from the donor structures, it can either be transported using static cold storage or using ex-vivo systems.
*Once all retrieval teams are in agreement, the aorta is cross-clamped for the heart and lungs to be retrieved, before the abdominal viscera are then retrieved

Figure 2 – A benched donor heart, about to be transplanted to the recipient
Recipient Procedure
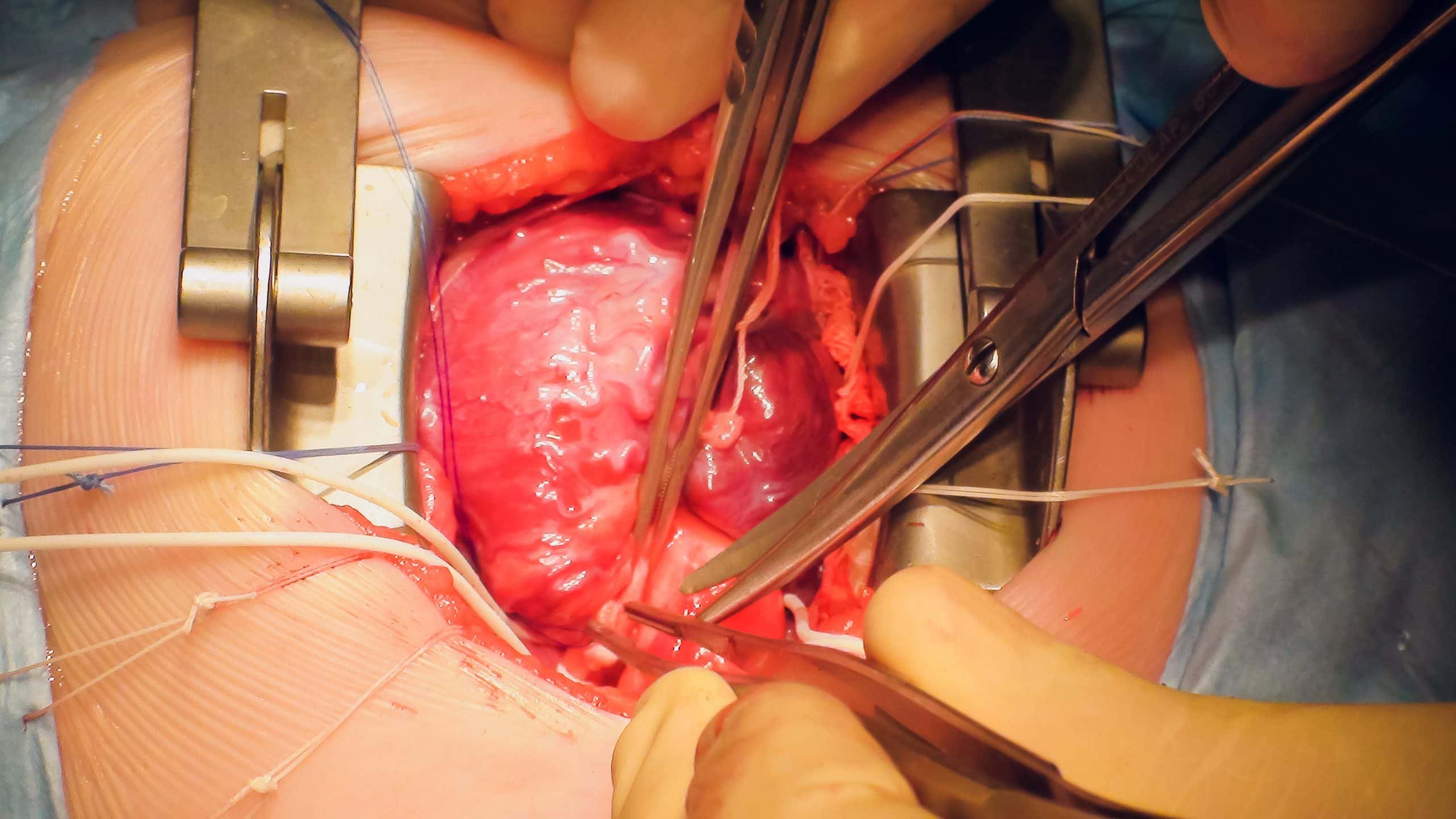
Once the donor heart is procured, the recipient will undergo a median sternotomy and the diseased heart is exposed. The recipient will be put onto cardiopulmonary bypass and the aortic cross-clamp will be applied.
The diseased heart will be excised just above the point at which the aorta meets the aortic valve and the pulmonary artery meets the pulmonary valve, and large tissue cuffs are preserved of the superior vena cava, inferior vena cava, and pulmonary veins.
Commonly the outflow tracts are anastomosed first, the aorta then the pulmonary artery, and then the superior and inferior vena cava can be anastomosed. The patient is then weaned from cardiopulmonary bypass and may require inotropic support and epicardial pacing wires. Protamine is administered to reverse the heparin effects and once haemostasis is achieved the chest is closed and drains left in-situ.
Complications
Early
Patients must be monitored for post-operative bleeding in the immediate post-operative period. Due to immunosuppressed status, post-operative infections are also common.
In the initial days following the procedure, patients are at risk of reperfusion injury and primary graft dysfunction. Ensuring good cardiac output is the priority in the initial phase, however often ECMO may be required during this period.
Late
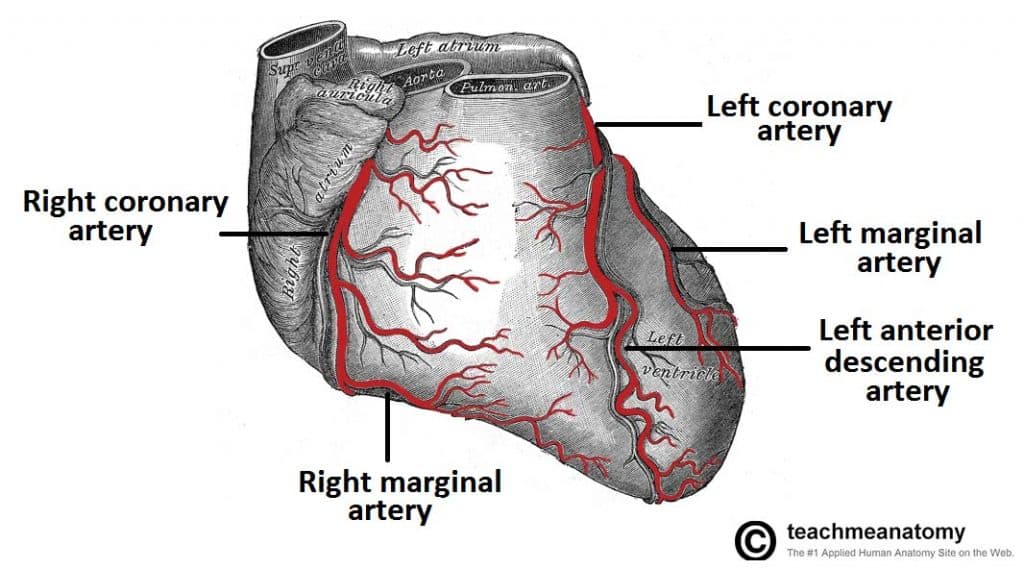
Heart transplant patients are at risk of cardiac allograft vasculopathy (narrowing of the coronary arteries), which typically occurs after the first 6 months. These patients require frequent follow-up angiography.*
Transplant patients require life-long immunosuppression, which is associated with increase risk of recurrent or atypical infections, nephrotoxicity, and certain malignancies (including post-transplant lymphoproliferative disorder).
Many patients will require temporary pacing post-operatively, and some go on to develop severe bradyarrhythmia requiring permanent pacemaker insertion (bradyarrhythmia may also be an early sign of rejection and must be investigated as such).
*The lack of autonomic innervation means patients are unable to always feel the symptoms of ischaemic heart disease
Key Points
- Heart transplantation is the final treatment option in end-stage heart failure
- Indications include ischaemic heart disease, valvular heart disease, cardiomyopathy (dilated, restrictive, or ischaemic), or congenital heart disease
- Heart transplants can occur alone or (rarely) as a combined procedure with a heart and lung transplantation