Introduction
Growth plate fractures are an important presentation in children and teenagers, and need urgent identification and appropriate management.
They are common fractures, accounting for around 35% of all skeletal injuries. The involvement of the physis (growth plate) means that any mismanagement can result in limb shortening or abnormal growth.

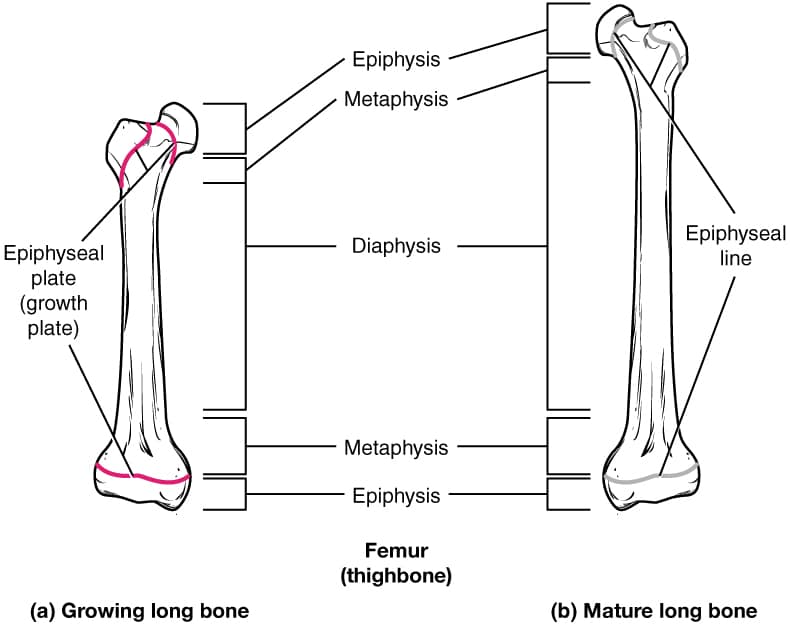
Figure 1 – A plain film radiograph showing a normal growth plate in a 12yr old patient
The Growth Plate
The growth plate consists of 3 parts, the epiphysis, physis and metaphysis. The physis is the hyaline cartilage plate found at each end of the long bones in children.
This is the site of endochondral ossification, where chondrocytes replace cartilage with bone, resulting in growth of the long bones. The growth plates normally close at the end of puberty, around 13-15yrs in females and 15-17yrs in males.
Clinical Features
Most growth plate fractures will occur following a fall or twist, however they can less commonly be caused by repetitive activities, such as gymnastics or running.
Patients with a growth plate fractures will usually present with pain at the affected site. Like most fractures, they will be unable to weight bear (if affecting the lower limb).
On examination, there may be bruising or swelling around the affected site, and with visible deformity at the fracture site in severe cases. Ensure to always assess (and document) the neurovascular status
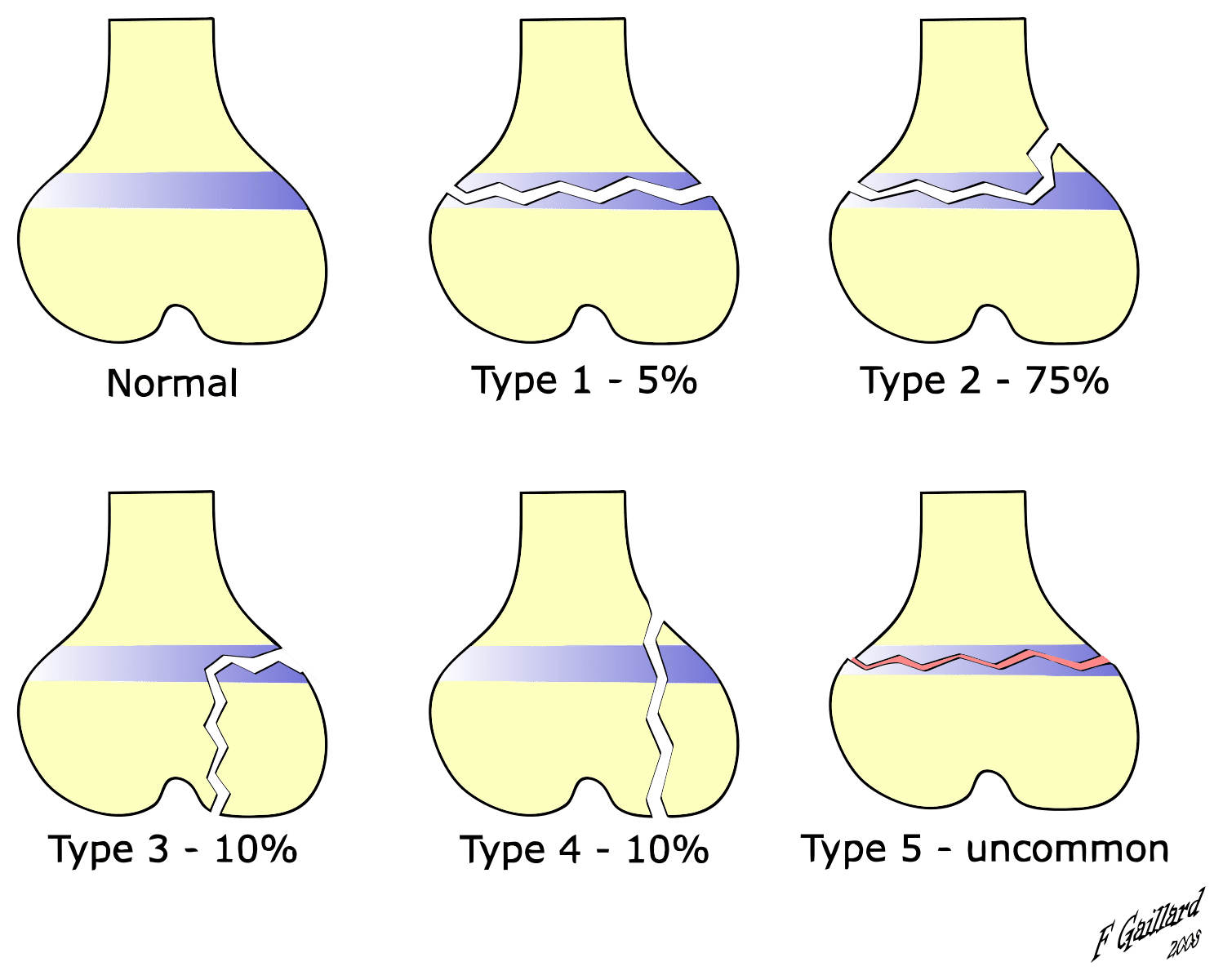
Salter-Harris Classification
Growth plate fractures are best classified using the Salter-Harris Classification (Fig. 3), useful to guide appropriate management and prognosis (the acronym SALTR is useful to remember the order):
- Type I – The fracture line is straight across the growth plate with no bone involvement; they often have a good prognosis (unless there is significant displacement of the epiphysis)
- Type II – The fracture line involves the growth plate and the bone above (i.e. the metaphysis); these are the most common type, making up 75% of all growth plate fractures
- Type III – The fracture line involves the growth plate and the bone below (the epiphysis); they often have a worse prognosis and may require surgical intervention
- Type IV – The fracture line passes through the whole growth plate, involving the metaphysis and epiphysis; they often have a worse prognosis and may require surgical intervention, due to involvement of the intra-articular surface
- Type V – There is a Crush injury of the growth plate, where compression is the mechanism of injury; these carry the worst prognosis, however are rare to occur (<1% of all growth plate fractures)
Investigations
All patients presenting with a suspected growth plate fracture require plain film radiographs (Fig. 4) for further assessment.
These should be taken in at least 2 views (e.g. antero-posterior and lateral), plus any additional region specific views depending on the injury location. Ensure to also image the joints above and below the region involved.
Further CT or MRI imaging may be required to inform operative planning or to assess the surrounding soft tissues.
Management
All patients presenting with traumatic injuries should be approached in an A to E manner, following ATLS principles. Ensure a full secondary survey is completed, to identify any further injuries or suspected fractures that may have been missed.
It is also important to assess for any potential safeguarding concerns, as with any paediatric injury that has occurred.
The management of growth plate fractures can be guided by the Salter-Harris Classification, however patient- and injury-specific factors will also influence definitive management chosen
Type I and II Fractures
Type I and II fractures are usually minimally displaced and good outcomes can be achieved with conservative management.
An acceptable closed reduction of the fracture seen on post-manipulation plain film radiograph can then be managed with immobilisation in a cast or splint, and review in orthopaedic fracture clinic in 7 days post-injury.
Children with growth plate fractures may present late; if more than 5 days after the injury, then manipulation should not be attempted and if not well-aligned, then operative intervention may be needed.
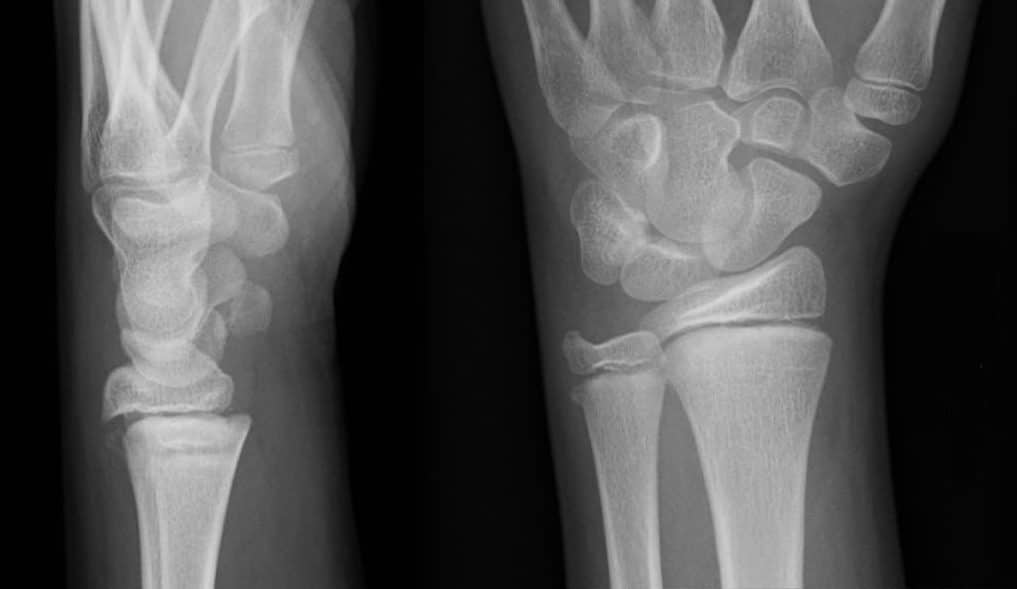
Figure 5 – Plain film radiograph showing a Salter-Harris type 1 of distal radius of a right wrist
Type III and IV Fractures
Type III and IV fractures are associated with greater displacement and instability. An anatomic reduction must be achieved as disruption of the intra-articular surface can lead to limited range of movement and function at that joint and early osteoarthritis.
Whilst closed reduction should be attempted, if unsuccessful there is a low threshold for open reduction and internal fixation (ORIF), given the instability in these fracture types
Type V Fractures
Type V fractures are the most difficult to manage. Most are diagnosed retrospectively when growth arrest or limb deformity has already occurred as a result of damage to the physis. Often referral to specialist centres is required.
Complications
The majority of growth plate fractures have a good prognosis and few patients experience long term complications.
However, in those cases where the fracture is missed or mis-managed, this can result in disruption or early closure of the growth plate, resulting in impaired function, growth arrest, or limb deformity.
Key Points
- Growth plate fractures are one of the most common skeletal injuries in children
- Approximately 75% are Type II fractures in the Salter Harris classification
- The mainstay of diagnosis required plain film radiographs only
- Type I and II may only require manipulation and immobilisation, whilst Type III and IV are more likely to require surgical management.
- Ensure patients receive follow up 7-10 days after treatment for repeat imaging