Introduction
Testicular cancer is most common cancer in males aged 20-40yrs, with those of Caucasian and Northern European descent at highest risk.
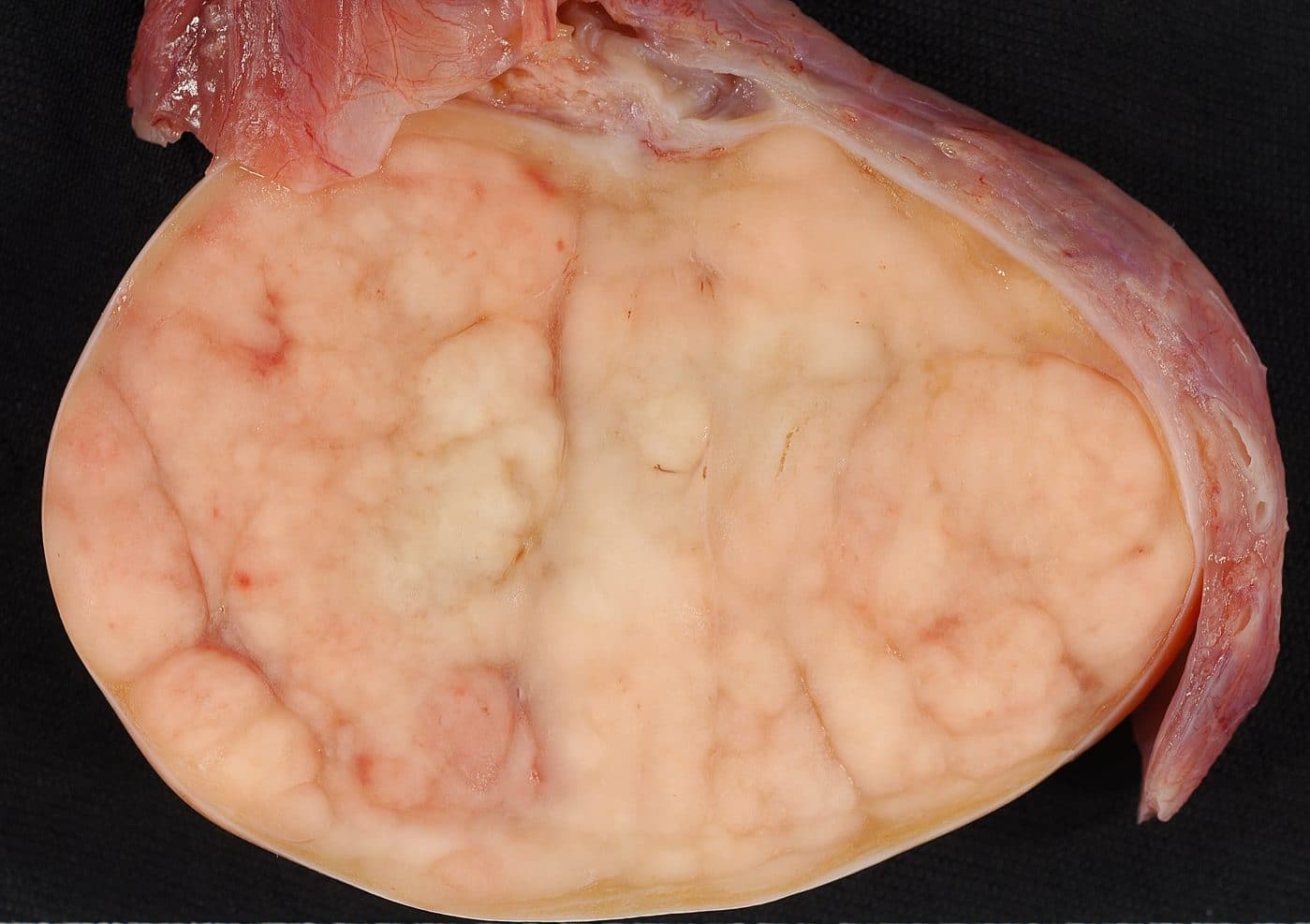
Primary testicular tumours are categorised into germ cell tumours (GCT) (95%) and non-germ cell tumours (NGCTs) (5%); GCTs can be further sub-classified into seminomas and non-seminomatous GCTs (NSGCT), and are usually malignant.
NGCTs are usually benign, comprising of either Leydig cell tumours or Sertoli cell tumours*. Seminomas tend to remain localised until late and have very good prognosis. NSGCTs include yolk sac tumours, choriocarcinoma, embryonal carcinoma, and teratoma; NSGCTs often metastasise early and have worse prognosis than seminomas.
*Leydig cell tumours and Sertoli cell tumours are benign and secrete androgens and oestrogens respectively
Risk Factors
Cryptorchidism (undescended testes) is associated with a 4-10x higher risk of GCTs. Other risk factors include previous testicular malignancy, a positive family history, Caucasian ethnicity, and Kleinfelter’s syndrome.
Clinical Features
Patients will present with a unilateral painless testicular lump. On examination*, the mass is typically irregular, firm, fixed, and does not transilluminate.
Evidence of metastasis may present with weight loss, back pain (from retroperitoneal metastases), or dyspnoea (secondary to lung metastases).
*Lymphatic drainage of the testes is to the para-aortic nodes, therefore localised lymphadenopathy may not be present, even in cases of metastatic disease
Differential Diagnosis
Differential diagnoses for a scrotal lump include epididymal cyst, haematoma, epididymitis, or hydrocoele.
Investigations
For patients with suspected cases of testicular cancer, tumour markers can be used for both diagnostic and prognostic* means. ßHCG is elevated in 60% of NSGCTs (100% in choriocarcinomas) and 5-10% of pure seminomas, whilst AFP can be raised in some NSGCTs but not in pure seminomas. LDH can also be used as a surrogate marker for tumour volume and necrosis, as well as for tumour response to oncological treatment.
Scrotal ultrasound (Fig. 3) should be used in the initial assessment of scrotal lumps, alongside concurrent tumour markers. The disease will then be staged via CT imaging with contrast of the chest-abdomen-pelvis.
Crucially, a trans-scrotal percutaneous biopsy should not be performed, as it might cause seeding of the cancer. Diagnosis is made through tumour markers and imaging alone.
*Levels can be used post-treatment to determine its efficacy
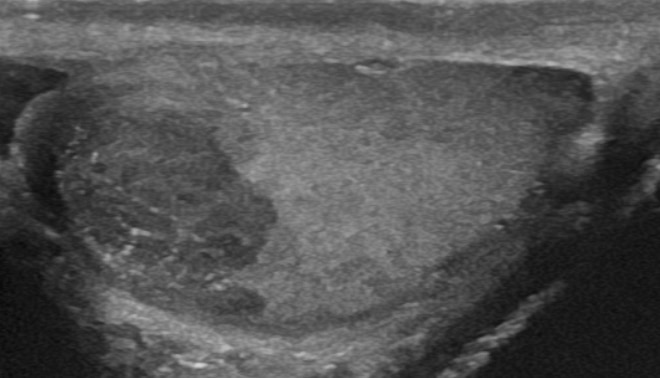
Figure 3 – US testes demonstrating a seminoma of the testis
Staging of Testicular Cancer
The Royal Marsden Classification can be used in the staging of the testicular cancer
| Stage | Characteristics |
|
I |
Disease confined to testes |
|
II |
Infra-diaphragmatic lymph node involvement |
|
III |
Supra- and infra-diaphragmatic lymph node involvement |
|
IV |
Extralymphatic metastatic spread |
Management
All patients with confirmed testicular cancer he should be discussed in a specialist MDT. The main treatment options for testicular cancer are surgery, radiotherapy, and chemotherapy; the treatment of choice depends on the tumour type, risk scoring, and prognosis.
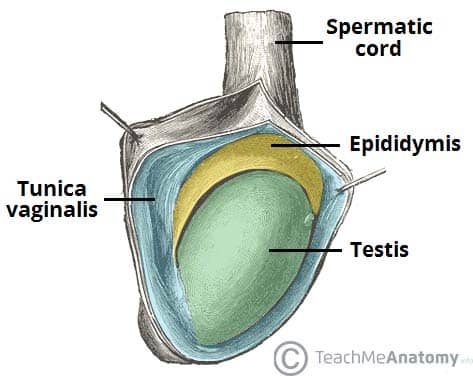
Most cases suitable for surgery will undergo an inguinal radical orchidectomy*. An inguinal approach (Fig. 4) allows for limited lymphatic disruption, important in cases of malignancy; the tumour-bearing testicle being removed with epididymis, spermatic fascia and cord.
Sperm abnormalities and Leydig cell dysfunction are frequently found in patients with testicular cancer prior to orchiectomy. Furthermore, chemotherapy and radiation treatment can additionally impair fertility. Therefore, in patients in the reproductive age group, pre-treatment fertility assessment should be performed, and semen analysis and cryopreservation offered to all patients.
*A biopsy of the contralateral testicle is performed in patients <40years old and the volume of contralateral testis <12ml, or there is a history of cryptorchidism or subfertility
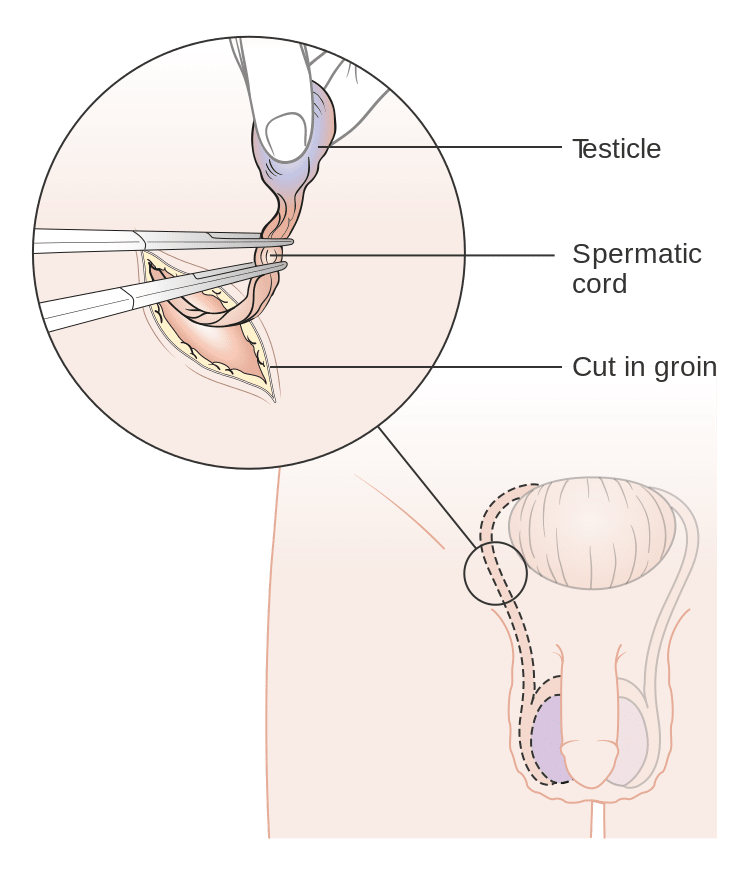
Figure 4 – Illustration demonstrating an inguinal approach for orchidectomy
Non-Seminomatous Germ Cell Tumours
Stage 1 NSGCTs will require orchidectomy, then further managed dependent on their risk score. Low risk patients without any evidence of vascular invasion can routinely enter just surveillance, whilst high risk patients (including embryonal cancer >50% or proliferation rate >70%) or those with vascular invasion require adjuvant chemotherapy, and then surveillance, including regular examination, surveillance CT imaging and plain film chest radiographs (CXRs), and tumour markers.
Metastatic NSGCTs management is also dependent on risk scoring. Cases with intermediate prognosis should be treated with chemotherapy, whilst those with poor prognosis should be treated with one cycle of chemotherapy before reassessment (those with marker decline should have continued chemotherapy cycles, whilst those with unfavourable decline should have their chemotherapy intensified).
Seminomas
Stage 1 seminoma can often be managed with orchidectomy alone and surveillance monitoring. Patients with a high relapse risk are often considered for adjuvant chemotherapy. Histological factors which indicate higher risk for relapse are invasion of rete testis and tumour size >4cm.
Surveillance for stage 1 seminoma includes twice yearly including regular examination, surveillance CT imaging, and tumour markers. Beyond 5 years, surveillance can be transferred to the GP, with regular examination and tumour markers alomne.
For metastatic seminoma, stage IIA can be treated with either radiotherapy or chemotherapy, whilst higher stage disease will require chemotherapy alone and treated similar to metastatic NSGCTs (as above).
Complications
Patients who under radiotherapy and chemotherapy often have an increased risk of secondary malignancies, such as leukaemia.
Prognosis of the disease depends on the tumour type and stage, however fortunately overall the condition has a high rate of complete remission. Of note, those with pure seminomas should be considered to have a good prognosis, with 5-year overall survival in patients with metastatic seminoma who receive treatment ranges from 88-95%.
Key Points
- Testicular cancer is most common cancer in males aged 20-40yrs
- Patients will present with a unilateral painless testicular lump
- Diagnosis is made through combination of tumour markers and imaging
- Management is dependent on tumour subtype, disease stage, and risk scoring