Introduction
Adhesive capsulitis (frozen shoulder) is a condition in which the glenohumeral joint capsule becomes contracted and adherent to the humeral head. This can result in shoulder pain and a reduced range of movement in the shoulder.
It affects approximately 3% of the population, it is more common in women, and peak onset is between 40-70yrs old. Those who have previously been affected by adhesive capsulitis are more susceptible to developing the condition in the contralateral shoulder.
Pathophysiology
Adhesive capsulitis may be categorised as primary or secondary:
- Primary adhesive capsulitis (idiopathic*)
- Secondary adhesive capsulitis – associated with rotator cuff tendinopathy, subacromial impingement syndrome, biceps tendinopathy, previous surgery or trauma, or known joint arthropathy
Adhesive capsulitis progresses in three stages: an initial painful stage, a freezing stage, and finally a thawing stage. However, there is little evidence to support the segregation of these phases, and that the pain associated with limitation in shoulder movement is often present throughout.
*Adhesive capsulitis is often associated with inflammatory diseases and currently theory suggests that it may have an autoimmune element

Figure 1 – The shoulder joint capsule in relation to the major bursae of the shoulder
Clinical Features
Patients will describe a generalised deep and constant pain of the shoulder (which may radiate to the bicep), that often disturbs sleep. Associated symptoms include joint stiffness and a reduction in joint function.
On examination, there may be a loss of arm swing and atrophy of the deltoid muscle. Generalised tenderness on palpation is common.
The patient will have a limited range of motion, mainly affecting external rotation and sometimes flexion of the shoulder (a full range of motion should prompt consideration of alternative differential diagnoses).
Differential Diagnosis
- Acromioclavicular pathology (e.g. acriomioclavicular joint injury, acromioclavicular arthritis, glenohumeral arthritis) – a more generalised pain may be present with weakness and stiffness related to pain
- Subacromial impingement syndrome (rotator cuff tendinopathy, subacromial bursitis) – may present with preserved passive movement and history of repetitive overuse/external compression of subacromial space risk factors
- Muscular tear (rotator cuff tear, long head of biceps tear) – the weakness often persists when the shoulder pain is relieved
- Autoimmune disease (polymyalgia rheumatica, rheumatoid arthritis, systemic lupus erythematous) – may present with a polyarthropathy and systemic symptoms
Investigations
The diagnosis of adhesive capsulitis is typically clinical, therefore can be made by clinical features alone. Plain film radiographs are generally unremarkable, but importantly can be used to rule out acromioclavicular pathology or atypical presentations of fractures.
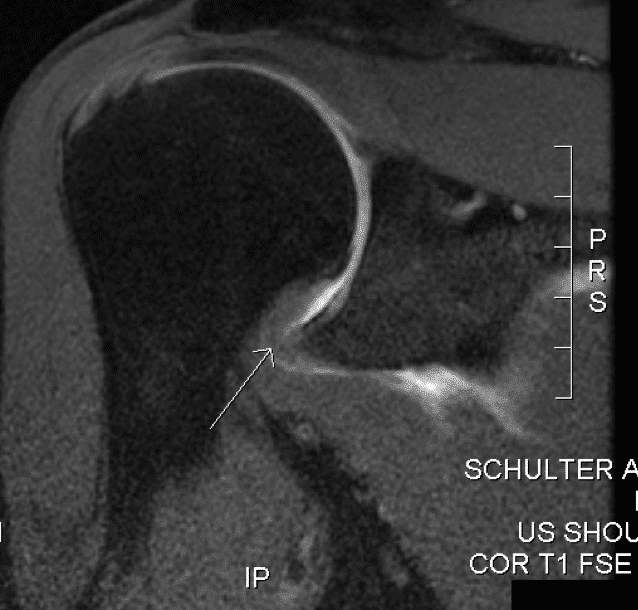
MRI imaging can reveal a thickening of the glenohumeral joint capsule in adhesive capsulitis (Fig. 2), but also can be used to rule out other conditions affecting the shoulder, such as subacromial impingement syndrome.
The condition is more common in diabetic patients, therefore for anyone presenting with adhesive capsulitis without any risk factors or precipitating events, checking the HbA1c and blood glucose measurements may be useful. It can also be associated with autoimmune thyroid disease and therefore measuring TSH levels can be indicated.
Management
Adhesive capsulitis is a self-limiting condition however recurrence is not uncommon. Recovery usually occurs over months to years and a proportion of patients will never recover full range of movement.
Initial management of the patient involves education and reassurance. Patients should be encouraged to keep active; all patients should receive physiotherapy and advice concerning appropriate shoulder exercises.
Management of pain initially begins with simple analgesics. Glenohumeral joint corticosteroid injections may be considered for those patients failing to improve.
Surgical Intervention
For patients with no improvement following prolonged engagement with full conservative treatment efforts and when symptoms significantly affect quality of life, surgical intervention may be considered.
Potential surgical interventions include joint manipulation under general anaesthetic to remove capsular adhesions to the humerus, arthrogaphic distension, or surgical release of the glenohumeral joint capsule.
Complications
A small proportion of patients will never regain a full range of motion but majority regain movement beyond that required to perform activities of daily living.
In some patients, the progression of symptoms may persist beyond two years and adhesive capsulitis may occur in the contralateral shoulder.
Key Points
- Adhesive capsulitis involves the glenohumeral joint capsule becoming contracted and adherent to the humeral head
- Patients presents with a generalised deep pain of the shoulder, associated with stiffness and a reduction in function
- Most diagnoses can be made clinically, however MRI imaging can be used to confirm the condition
- Adhesive capsulitis is a self-limiting condition, management is typically conservative and rarely requires surgical intervention