Introduction
Tinnitus is the perception of sound in the absence of an external auditory stimulus. Sounds heard can be intermittent or continuous, and have been described as variety of sounds (e.g. ringing, buzzing, humming, whistling, or clicking).
The condition is common and affects around 10% of the population, with severe cases having a significant detrimental impact on quality of life. Most of the cases are of idiopathic cause.
Pathophysiology
The pathophysiology of tinnitus is not well understood. Current theories suggest it comes from abnormal neuronal activity along the auditory pathway, originating anywhere along the auditory pathway.
Tinnitus can be classified as primary or secondary:
- Primary – no underlying cause is identified, often associated with sensorineural hearing loss
- Secondary – an underlying cause has been identified, often further sub-classified into subjective (only heard by the patient) or objective (also audible to the examiner)
Tinnitus can also be classified into pulsatile (noises synchronous with patient’s pulse) or non-pulsatile.
Causes of Tinnitus
- Otological (conductive), e.g. cerumen impaction, otosclerosis, otitis media
- Otological (sensorineural), e.g. presbycusis, Meniere’s disease
- Medications, e.g. NSAIDs, tetracyclines, quinine, sodium valproate, chemotherapy
- Metabolic, e.g. hyperthyroidism, zinc deficiency
- Neurological, e.g. acoustic neuroma, multiple sclerosis
- Musculoskeletal, e.g. TMJ dysfunction, tensor tympani, stapedius myoclonus
- Psychological, e.g. anxiety, depression
- Vascular, e.g. glomus jugulare, arterio-venous malformations, intracranial hypertension
Clinical Features
Tinnitus will present in a variety of ways dependent on the underlying cause, hence it is important to clarify certain features, including duration, character, laterality, and associated symptoms (including hearing loss and focal neurology). Patients with unilateral tinnitus should have further investigations performed.
On examination, otoscopy and audiometry are essential. Examine the cranial nerves and TMJ routinely for focal neurology.
Specifically, in pulsatile tinnitus, auscultation of the temporal bone with a stethoscope can identify a dual fistula in those with an underlying vascular malformation.
Tinnitus as Otological Emergency
Current NICE guidelines recommend that patients presenting with tinnitus should be referred as an otologic emergency if they have features of:
- Sudden onset pulsatile tinnitus
- Significant neurology
- Severe vertigo
- Secondary to head trauma
- Unexplained sudden hearing loss
Investigations
All patients presenting with tinnitus, particularly those with symptoms persisting for greater than six months, should be referred for comprehensive audiological assessment. Such assessments include pure-tone audiometry (PTA) and tympanometry; patients’ blood pressure should be recorded as well.
Most cases should have non-urgent blood tests sent, including full blood count, thyroid function tests (TFTs), lipid levels, and/or blood glucose (random or fasting).
Routine imaging of the head and neck is not recommended. However, if there is persistent unilateral pulsatile tinnitus CT imaging with contrast will be indicated. MRI imaging of the internal acoustic meatus will be considered for persistent unilateral tinnitus to rule out cerebellopontine angle lesions, especially if associated with unilateral sensorineural hearing loss.
Management
For the vast majority of affected, conservative management and reassurance is all that is required. Tinnitus is usually mild and will self-resolve over time.
If an underlying cause is identified, this should be managed accordingly. For primary case, the focus of management is mainly centred on habituation to the symptoms*. Tinnitus retraining therapy (TRT) and cognitive behavioural therapy (CBT) have both also been shown to be effective at reducing the impact of tinnitus.
As tinnitus is often accentuated in quiet environments, patients with concurrent hearing loss have been shown to benefit from the use of hearing aids. In some cases, tinnitus-masking devices are available which emit a constant, low-level white noise which help to distract patients.
There is a limited role for surgery in the treatment of tinnitus.
*No pharmacological treatments are recommended at present for the treatment of tinnitus
Acoustic Neuroma
Acoustic neuromas, also termed vestibular schwannomas, are benign tumours that arise from the Schwann cells surrounding the vestibulocochlear nerve (CN VIII).
The vestibular portion of the nerve is most commonly affected and account for 8% of all brain tumours (specifically 80% of tumours at the cerebellopontine angle, Fig. 3)
Acoustic neuromas derive due to abnormalities in tumour suppressor genes on chromosome p22. Bilateral vestibular schwannomas are rare and often associated with neurofibromatosis type 2
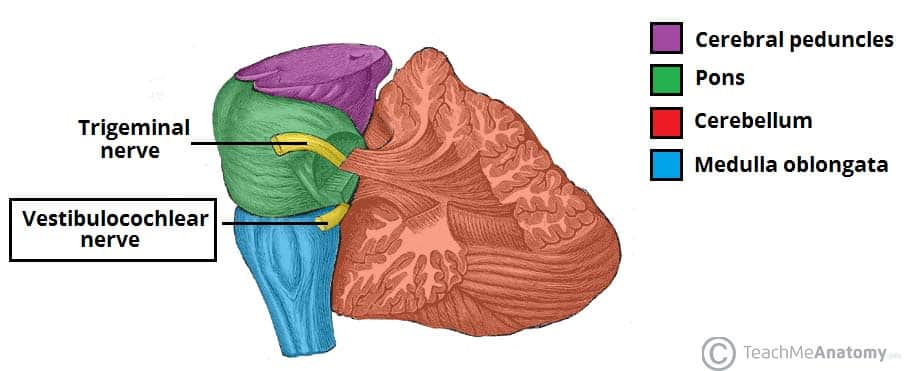
Figure 3 – The origin of the vestibulocochlear nerve from the cerebellopontine angle
Clinical Features
The classic triad is that of progressive unilateral sensorineural hearing loss, tinnitus, and vertigo, however patients commonly present with only one or two of these symptoms*.
Progressively enlarging tumours may cause features similar to that of any space occupying lesions, including cranial nerve palsy, headaches, seizures and reduced consciousness (very rare as the lesion is usually slow growing)
*Most cases will present with unilateral sensorineural hearing loss alone initially
Investigations
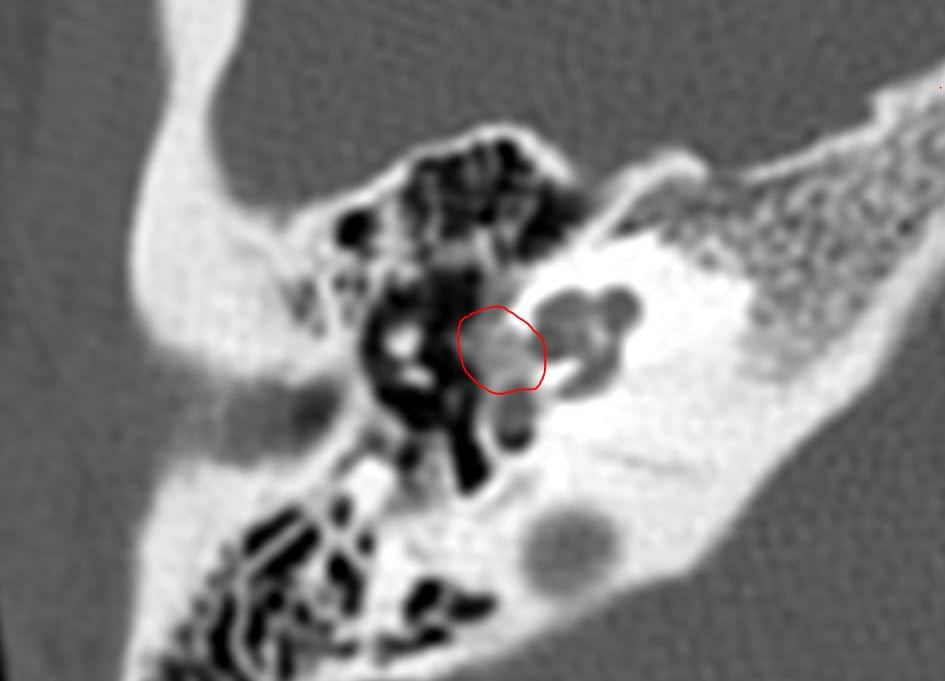
An MRI scan with contrast of the internal auditory meatus (IAM, Fig. 4) is the gold standard for imaging suspected vestibular schwannomas*. All patients with unexplained sudden sensorineural hearing loss should have an MRI IAM requested.
*Tumours arising from within the internal acoustic canal that expand into the CPA are often described as having an “ice-cream cone” appearance
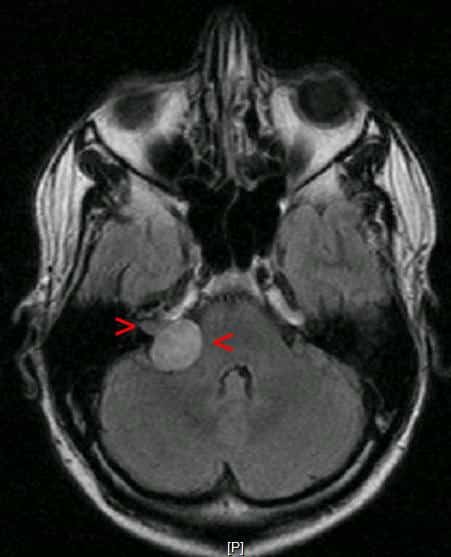
Figure 4 – An acoustic neuroma as seen on an MRI IAM scan
Management
Acoustic neuromas are typically slow growing (2-3mm per year), therefore monitoring interval MRI scanning can be done for patients with small tumours, limited clinical signs, or in patients with significant co-morbidities (Table 1).
Stereotactic radiosurgery involves focal collimation of gamma rays to slow or stop tumour growth. This method tends to produce good tumour control, with high rates of hearing and facial nerve preservation.
Surgical technique includes translabyrinthine, middle fossa, or retrosigmoid approaches, with the aim of surgery being for total removal of the tumour. Subtotal resection is often accepted where complete removal would lead to facial nerve compromise (and any remaining bulk managed with interval MRI scanning or radiosurgery if indicated).
Surgical management for acoustic neuroma is often reserved for large tumours due to potential complications from surgery and management is based on the recommendation of the skull base MDT (a combination of neurosurgery and otological skull base surgeons).
| Size of Tumour | Management |
| Small (<1.5cm) |
|
| Medium (1.5cm – 3cm) |
|
| Large (>3cm) |
|
Table 1 – Management for Patients with Acoustic Neuroma
Key Points
- Tinnitus is the perception of sound in the absence of an external auditory stimulus
- Most cases can be managed conservatively however there are a few red flags to be aware of that warrant an urgent referral
- Acoustic neuromas classically present with a triad of unilateral sensorineural hearing loss, tinnitus, and vertigo, and should be investigated with an MRI IAM with contrast
- Conservative measure for tinnitus management includes distraction sound, masking techniques, and tinnitus therapy
- Acoustic neuromas are very slow-growing benign tumours and management should involve a skull base MDT
- Acoustic neuroma management depends on its size, with small ones suitable for continuous surveillance and larger ones for surgical resection or stereotactic radiosurgery