This article is for educational purposes only. It should not be used as a template for consenting patients. The person obtaining consent should have clear knowledge of the procedure and the potential risks and complications. Always refer to your local or national guidelines, and the applicable and appropriate law in your jurisdiction governing patient consent.
Overview of Procedure
A diagnostic laparoscopy is a minimally invasive procedure that allows direct visualisation of the intra-abdominal organs.
It is mainly performed for in the investigation of acute abdominal pain of uncertain aetiology, allowing therapeutic interventions to subsequently take place as appropriate, most commonly for appendicitis. It can also be performed in stable trauma patients with penetrating injuries or in the staging of intra-abdominal cancers (including obtaining tissue for histological diagnosis e.g. peritoneal fluid for cytology or peritoneal biopsy).
Laparoscopy is associated with shorter post-operative recovery, lower pain scores, and reduced rate of wound infections compared to open exploratory surgery.
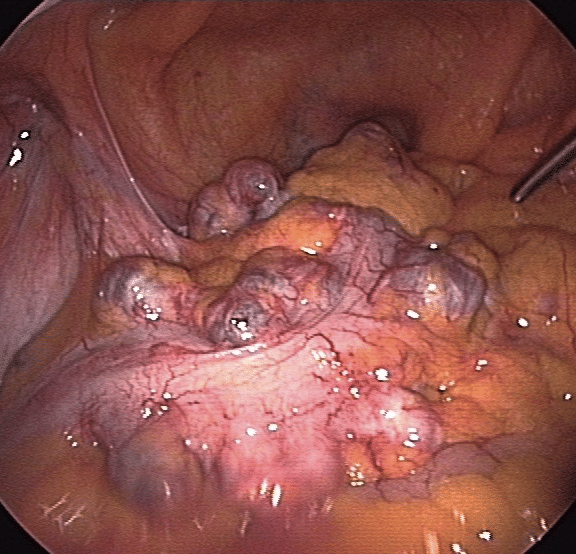
Figure 1 – Laparoscopic view of diverticula in the sigmoid colon
Complications
Intra-Operative
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Haemorrhage | Port insertion can damage any intra-abdominal organ, including the abdominal aorta; also be aware of the inferior epigastric artery when inserting ports into the left or right iliac fossa | Direct visualisation of additional ports during insertion |
| Injury to surrounding structures including bowel, bladder, ureter, liver, and spleen | A laparoscopy involves assessing all organs, which can be damaged in the process | Decompress the bladder with a catheter prior to the procedure |
| Conversion to open surgery including full laparotomy* | This may be necessary if the procedure is difficult or there is other pathology, such as a malignancy that may require open resection | |
| Stoma | This is rare, particularly in young patients, but it may be required in a select cases if a bowel resection is required | |
| Anaesthetic Risks | Includes damage to the teeth, throat and larynx, reaction to medications, nausea and vomiting, cardiovascular and respiratory complications | Forms a part of the anaesthetist assessment before the operation |
*This is not a true complication, merely a consequence of difficult pathology, but always should be included
Early
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Pain | The patient will have local anaesthesia into the wounds and simple analgesia post-operatively | |
| Bleeding | There is a small chance of bleeding and bruising in the abdomen post-surgery | |
| Infection | Superficial wound infection is possible, however collections in the pelvis or paracolic gutters can also occur | Peri-operative antibiotics will reduce the risk of wound infections |
| Scarring | Any scar may form a keloid scar, particular in high-risk ethnicities | |
| Blood Clots | DVTs and PEs are a possibility in any operation; the risk is increased in patients with a raised BMI, on the contraceptive pill, previous DVT, pregnancy, current smokers, or known malignancy | The patient will be given anti-embolism stockings and low molecular weight heparin peri-operatively to minimise this risk as deemed appropriate |
| Stroke, MI, Kidney Failure, Death | Although small, this is always a risk in any major surgery |
Late
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Hernia | Any incision involving the abdominal wall has the potential to cause a hernia in future, either through a port site or in open surgery. | Avoid heavy lifting and straining for 6 weeks post-surgery |
| Adhesions | Any abdominal surgery may cause adhesions as a reaction to the procedure, however laparoscopic surgery is lower risk than open surgery | |
| Further surgery | Depending on the intra-operative findings, the patient may require further procedures for definitive management |
