Introduction
Going into theatre for the first time can be unnerving. The operating room is a fast-paced and often serious environment with many different professional groups working within it. Without a particular set of rules and behaviour standards, it would not function as efficiently as it does.
Due to this, it can be a particularly daunting place to be when you are not sure what might be happening or what you should do in order to be a productive member of the team.
Whether you are a student starting your first surgical rotation or are a surgical trainee wanting to refresh the essentials, this article will serve as a one-stop guide to theatre etiquette.
The Operating Room Layout
Different hospitals and surgical departments will have a different theatre layout but all have common components.
There are several parts to the operating theatre:
- Scrubbing area – contains sinks and sterile gowns, gloves, and masks/visors, and any other specialised equipment needed to scrub up for the operation
- Operating room – where the main part of the surgical operation occurs, containing the operating table, theatre lights, anaesthetic equipment, and the scrub nurse table
- Anaesthetic room – where the anaesthesia is often administered, especially for general or regional anaesthesia
- Storage area – contains the supplies of the equipment required for the operation, also are often sterile
Many theatres have a specific door to enter through, especially once the operation has started. Look for the notices on the theatre door and if there is one that says “do not enter through this door” then do avoid this route and find an alternative.
The set-up of the operating room will vary hugely depending on the operation being performed (see Fig. 1).
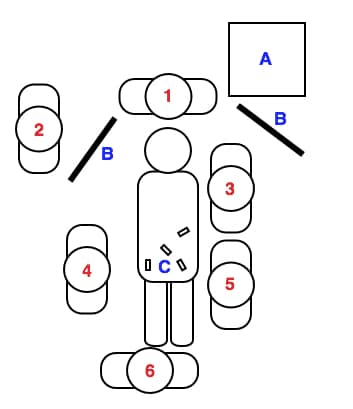
Figure 1 – set-up outline for typical laparoscopic cholecystectomy; 1 = anaesthetist(s), 2 = circulating nurse, 3= camera holding surgeon, 4 = assistant surgeon, 5 = primary surgeon; 6 = scrub nurse; A = anaesthetic machine, B = laparoscopic camera monitor, C = laparoscopic ports
Roles of the Theatre Staff
There are many different staff present in theatre, even for the more “routine” operations, and all work together to ensure a successful operation and patient safety.
The operating theatre can be a busy place with other members of staff, visitors, and students*. The below list is not an exhaustive list of all those present but gives an outline of those who are likely to be present:
- Anaesthetist
- Responsible for anaesthetic induction and physiological monitoring peri-operatively
- Scrub Nurses
- Can either be qualified nurses who have subspecialised to work within theatres or Operating Department Practitioners (ODPs)
- Work directly with the surgeon within the sterile field, looking after the surgical equipment required for the procedure and handing them to the surgeon when required
- Surgeon
- Performs the procedure, this may be working on their own or with one or more assistant present
- Operating Department Practitioners
- Trained healthcare professionals in the peri-operative environment, work as part of the scrub or circulating team and with the anaesthetist to support the operating team
- Recovery Nurses
- Qualified nurses who provide critical care after surgery, monitoring the progress of the patients’ condition until stable to return to the ward environment
*Many hospitals now use different colour scrub hats for role recognition and there should be guides on the wall as to which one you should wear, allowing for quick role recognition within the operating theatre
How to Approach the Operating Room
Before entering the theatre department, it is important that you change into scrubs, have suitable footwear, and wear an appropriate scrub cap.
Arrive early and ensure to introduce yourself to the surgical team, especially the surgical nurse in charge; ask for permission to shadow or scrub in for the surgery. Make sure to write your name down on the theatre attendance list and on the board (if present).
It is always good practice to read up on the patient (especially the medical history, the diagnosis, and planned procedure) before the surgery. You might be asked questions during the procedure and you will get far more out of the operation if you know why it is being done in the first place.
If you are unsure how to scrub up, ask a theatre nurse or an ODP to show you how to do it properly if they have free moment. Be respectful during the surgery however also show keenness and proactivity where appropriate. And above all, enjoy the experience!
Tips from the Experts
Mr Ayoola Awopetu (Vascular Surgery Registrar, Cambridge University Hospitals)
“Always make friends with the scrub nurses. Remember, the consultant has worked with the nurse for several years, you’ve been there for a few hours”
Ms Suzanne Biers (Consultant Urological Surgeon, Cambridge University Hospitals)
“Attend the ward to shadow the surgical team taking consent, showing you are motivated and interested, as well as the learning opportunity available, particularly about the potential complications. Also remember to bring your own clogs to theatres (and spare socks if you are involved in urology cases).”
Professor Henry Pau (Consultant ENT Surgeon, University Hospitals of Leicester)
“Do not touch anything green or blue unless you are scrubbed as things that are placed on green or blue towels are likely to be sterile”
Key Points
- Read up on the indications for the operation the night before and ensure take a brief history from the patient before the operation
- Ensure you enter through the correct doors and look through the window before you walk in
- Always stay at the end and help move the patient if required
- Be polite and friendly, theatres are usually supportive and friendly environments
