Introduction
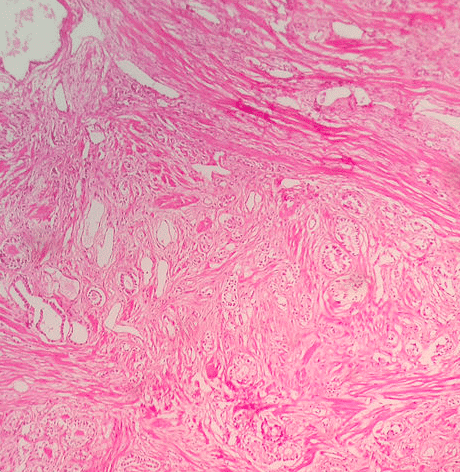
Benign prostate enlargement (BPE) is an enlargement of the prostate gland which is most often due to benign prostatic hyperplasia (BPH). BPH is a histological diagnosis and is characterised by non-cancerous hyperplasia of the glandular-epithelial and stromal tissue of the prostate leading to an increase in its size.
BPH is very common and the risk increases with age; approximately 40% of men over 50 years have evidence of enlargement, rising to 90% of men over 80 years.
BPH is the most common cause of Bladder Outlet Obstruction in men and hence can be considered the most common cause of Lower Urinary Tract Symptoms (LUTS) in men*.
*It is important to note that 15-30% of men over 65 have LUTS regardless of BPH
Pathophysiology
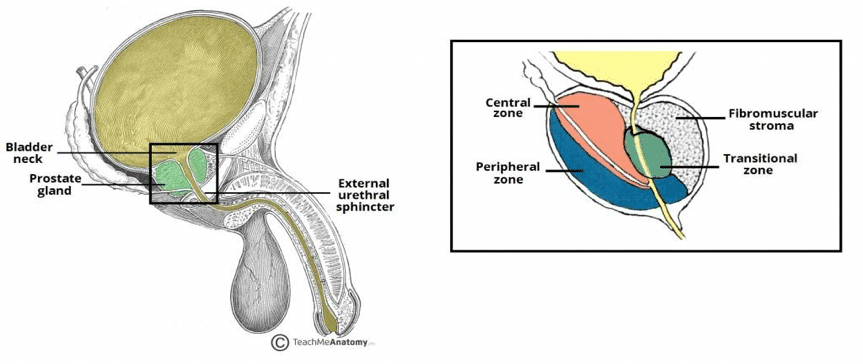
The prostate is a gland found in the male reproductive system which produces prostatic fluid.
The exact mechanism of benign prostatic hyperplasia has not been identified. However, it is clear that androgens play a role particularly in the development in the gland during adolescence and the future development of BPH.
Unlike other androgen dependent organs in the body, the prostate converts testosterone to dihydrotestosterone (DHT) using the enzyme 5α-reductase. DHT is more potent and accounts for 90% of androgen in the tissue. Also, unlike other tissues, the prostate retains the ability to respond to testosterone and thus levels of DHT also remain high though life.
Risk Factors
Age is the primary risk factor for developing BPH. Other risk factors include family history (first degree relatives), black African or Caribbean ethnicity, and obesity
Clinical Features
Patients with benign prostatic hyperplasia will generally present to primary care with lower urinary tract symptoms (LUTS), often predominantly voiding symptoms (hesitancy, weak stream, terminal dribbling, or incomplete emptying), accompanied by storage symptoms (urinary frequency, nocturia, nocturnal enuresis, or urge incontinence). Other less common symptoms can include haematuria and haematospermia.
A Digital Rectal Examination (DRE) is essential in order to help distinguish BPH from prostate cancer. A firm, smooth, symmetrical prostate is a reassuring sign (a more rounded prostate of greater than two finger widths may indicate enlargement). As part of the initial assessment, every patient should also complete an International Prostate Symptom Score (IPSS) questionnaire.
The International Prostate Symptom Score
The IPSS is a validated screening tool used in the evaluation and quantification of LUTS.
A score of 0-5, with 0 being ‘never’ and 5 being ‘almost always’, is assigned by the patient to each of the following questions. Scores of 0-7 are mild, 8-19 moderate and 20+ severe.
Each question begins with “Over the past month how often have you…”. More details can be found on the British Association of Urological Surgeons (link here)
Differential Diagnosis
Common differential diagnoses for benign prostatic hyperplasia include:
- Prostate cancer – patients may present with LUTS, however an asymmetrical craggy/nodular prostate and raised PSA are indicative of prostate cancer
- Urinary Tract Infection – the addition of dysuria, loin or suprapubic pain, or pyrexia, in the presence of a nitrite and/or leucocyte positive urine dip
- Overactive bladder – although the patient will present with LUTS, storage LUTS will predominate; additionally, patients with just overactive bladder will have a good flow rate (max flow QMax >20ml/s)
- Bladder cancer – haematuria is likely to be the predominant feature, LUTS are less common (especially initially)
Investigations
A urinary frequency and volume chart should be completed by all patients with bothersome LUTS. Bedside urinalysis should always be performed to exclude urinary tract infection. A post-void bladder scan can be helpful in assessing any significant chronic retention present
All men over the age of 50yrs (40yrs in black African or Caribbean men) presenting with LUTS for the first time, should be counselled for a PSA test.
Further Investigations
An ultrasound scan of the renal tract can also be used to calculate the volume of the prostate* alongside assessment of the rest of the renal tract for urinary retention or hydronephrosis. Any prostate >30ml (volume calculated by width x height x length x 0.52) is deemed enlarged.
Urodynamic studies is used in selected cases where the diagnosis is not certain or there is concern for detrusor failure. It can give objective measurements related to reported symptoms, including bladder contractility, flow rate, and storage capacity. The bladder outlet obstruction index (BOOI) can help diagnose obstructive voiding related to BPH*.
*Calculated using maxium flow rate (Qmax) and detrusor pressure at maximum flow rate (Pdet max); BOOI = Pdet max – (2 x Qmax). A BOOI >40 = obstructed, BOOI 20-40 = equivocal, and BOOI <20 = unobstructed

Figure 3 – Hydronephrosis with associated cortical atrophy, which can be seen in long-standing cases of high-pressure chronic retention secondary to BPH
Management
For patients who have an incidental identification of benign prostatic hyperplasia, with no clinical features of the condition nor of any significant complications, many patients can simply be reassured and advised BPH is not a cause for significant concern.
Asking patients to keep a symptom diary, providing a medication review (especially iatrogenic causes of LUTS), and giving suitable lifestyle advice (e.g. moderating caffeine and alcohol intake) are helpful conservative options that can be done for all patients.
Medical Management
Most men with symptomatic BPH should initially be trialled on an α-adrenoreceptor antagonist (α-blockers)*, such as tamsulosin. They act by relaxing prostatic smooth muscle via blockade of α-adrenoceptors, thus reducing the dynamic component.
They provide a symptomatic benefit within a few days* and their response rate to this treatment is thought to be around 30-40%; those who do respond can expect approximately a 4-point improvement in their IPSS.
*Significant side effects are associated with alpha blockers, such as postural hypotension, retrograde ejaculation, and Floppy Iris Syndrome (occurs intra-operatively in those undergoing cataract surgery).
For those that remain symptomatic despite α-adrenoreceptor antagonists, 5α-reductase inhibitors, such as Finasteride, are often then trialled*. They act to prevent the conversion of testosterone to DHT, resulting in a decrease in prostatic volume. In patients with erectile dysfunction, PDE5 inhibitors can be trialled and if there are severe storage LUTS consider an anti-cholinergic (avoid when high post-void residuals noted).
*Due to the mechanism of action, it can take up to six months to perceive symptomatic benefit from the use of 5α-reductase inhibitors
Surgical Management
Patients who are refractory to medical management or develop a significant sequlae of BPH (e.g. high pressure retention) will be referred for potential surgical management. Various surgical procedures are available, ranging from minimally invasive (Rezum/Steam treatment and UroLift) to more invasive (TURP procedure, GreenLight PVP, and HOLEP procedure).
A TransUrethral Resection of the Prostate (TURP) is the most widely used procedure undertaken to manage BPH (FIg. 4), involving endoscopic removal of obstructive prostate tissue using a diathermy loop to increase the urethral lumen size. It has excellent clinical outcomes, many patients having significant clinical improvement within a few months. Complications of TURP include TUR syndrome, haemorrhage, sexual dysfunction, retrograde ejaculation, and urethral stricture.
TURP Syndrome
TURP syndrome (aka TUR syndrome) is a rare but potentially life-threatening complication of TURP. TURP using monopolar energy requires use of hypoosmolar irrigation during the procedure which can result in significant fluid overload and dilutional hyponatremia as the fluid enters the circulation through the exposed venous beds.
Patients with TURP syndrome present with confusion, nausea, agitation, or visual changes and needs urgent management by addressing the fluid overload and carefully reducing the level of hyponatremia. Use of glycine as the irrigating agent can lead to further neurological issues as it can act as an inhibitory neurotransmitter.
Fortunately, TURP syndrome is increasingly rare due to the use of bipolar energy which uses isotonic irrigation fluids.
A Holmium Laser Enucleation of the Prostate (HoLEP) procedure involves using a Holmium:YAG laser used to heat and dissect sections of prostate into the bladder. It is becoming increasing more prevalent in use due to excellent outcomes and reduced post-operative complications, its use only being limited due to it being a technically challenging procedure.
Although used less commonly, simple prostatectomy using open or minimally invasive surgical techniques remain an option for patients with large prostates.
Prostate artery embolisation can also be considered but is generally reserved for patients not suitable for surgical options who have a considerable effect to their quality of life or complications from BPH such as chronic retention or bleeding.
Complications
The main complication of BPH is high-pressure retention, where chronic or acute-on-chronic urinary retention results in a post-renal kidney injury. Other complications of the condition include recurrent urinary tract infections or significant haematuria episodes.
Key Points
- Benign prostatic hyperplasia is very common and the risk of the condition increases with age
- Urinary flow rate and post-void residual scans can be used in objectively assessing urinary symptoms
- All patients should be offered advice on lifestyle and discussion of conservative management options
- There are a vast array of both medical and surgical management options available