Introduction
Renal tract stones (also termed urolithiasis) are a common condition, affecting around 2-3% of the Western population. They are more common in males and typically affect those <65yrs. They commonly form as renal stones (within the kidney) but can migrate to become ureteric stones (within the ureter).
Around 80% of urinary tract stones are made of calcium, as either calcium oxalate (35%), calcium phosphate (10%), or mixed oxalate and phosphate (35%). The remaining stone compositions include struvite stones* (magnesium ammonium phosphate), urate stones (the only radiolucent stones), and cystine stones (typically associated with familial disorders affecting cystine metabolism).
*Struvite stones are often large soft stones, the most common cause of “staghorn calculi” (Fig. 1), whereby the stone will fill the renal pelvis

Figure 1 – A large staghorn calculi, as seen on plain film abdominal radiograph
Pathophysiology
The basis for formation of urinary tract stones is over-saturation of urine. Calcium and oxalate precipitate at lower saturation levels and are therefore the most common stone composition.
However, certain stone types that form may also be caused by a specific underlying pathology.
For struvite stones, also called infection stones, form in alkaline urine in the presence of urease-producing organisms, such as Proteus and Klebisella species. Urease catalyses urea into carbon dioxide and ammonia, which leads to the precipitation of magnesium ammonium phosphate crystals.
For urate stones, high levels of purine in the blood, either from diet (e.g. red meats) or through haematological disorders (such as myeloproliferative disease), results in increase of urate formation and subsequent crystallisation in the urine.
For cystine stones, these are typically associated with homocystinuria, an inherited defect that affects the absorption and transport of cystine in the bowel and kidneys; as citrate is a stone inhibitor, hypocitraturia from the condition can thus predispose affected individuals to recurrent stone formation.
Location of Ureteric Stones
For stones that enter the drainage system of the urinary tract, there are three natural narrowed points where stones are likely to impact:
- Pelviureteric Junction (PUJ), where the renal pelvis becomes the ureter
- Crossing the pelvic brim, where the iliac vessels travel across the ureter in the pelvis
- Vesicoureteric Junction (VUJ), where the ureter enters the bladder
Clinical Features
The most common presenting symptom of ureteric stone is pain*, termed ureteric/renal colic, which occurs from the increased peristalsis from around the site of obstruction. The pain has a sudden onset, severe, and radiates from flank to pelvis (termed “loin to groin”), often associated with nausea and vomiting.
Distal ureteric stones may cause urinary frequency or need to micturate (despite an empty bladder). Haematuria occurs in around 90% cases, however this is typically non-visible. In certain cases, renal calculi can become infected, therefore associated symptoms, such as rigors, fevers, or lethargy. may be present; in severe cases, patient’s may shown clinical features of sepsis.
Examination is typically unremarkable, occasionally demonstrating some tenderness in the affected flank. There may be signs of dehydration, from reduced fluid intake secondary to associated vomiting.
*It is possible to have no pain with a stone, especially if the stone is non-obstructing
Differential Diagnosis
Differentials for flank pain include pyelonephritis, ruptured AAA, biliary pathology, bowel obstruction, lower lobe pneumonia, or musculoskeletal related pain.
Investigations
A urine dip can show microscopic haematuria, as well as evidence of infection (always ensure to send a urine culture as well in such cases).
Routine bloods should be performed, include FBC & CRP (for evidence of infection) and U&Es (to assess renal function). Urate and calcium levels can also aid in the assessment of stone analysis; if the patient notices they have passed the stone during micturition, retrieval of the stone and sending for analysis can also be of use.
Imaging
The gold standard for diagnosis of renal stones is a non-contrast CT scan of the renal tract (KUB). The benefit of the CT KUB (Fig. 3) as an imaging modality is the high sensitivity and specificity in identifying stone disease, as well as concurrent assessment of any alternative pathology.
Ultrasound scans of the renal tract can often be used concurrently in cases of known stone disease, to assess for any hydronephrosis (they can also often detect renal stones, however not ureteric stones). Its benefits are in no radiation risk, however are often operator dependent.
Plain film abdominal radiographs (AXR) are rarely used for the initial assessment of stone disease, as not all stones are radio-opaque which limits their use, alongside their associated radiation exposure. However, if a patient is known to have radio-opaque urinary tract calculi an AXR may be used as part of stone surveillance.
Management
Initial Management
Patients with renal stones will often be dehydrated, secondary to reduced oral fluid intake +/- vomiting, so ensure adequate fluid resuscitation if required.
For the majority of cases, renal stones will pass spontaneously without further intervention*, especially if in the distal ureter or <5mm in diameter. Ensuring patients have sufficient analgesia is paramount (NSAIDs per rectum are the most effective).
Any evidence of significant infection or sepsis present warrants intravenous antibiotic therapy and urgent referral to the urology team.
*Alpha receptor antagonists, such as Tamsulosin, are not routinely used for ureteric stones – there is limited evidence that their use may be beneficial in distal ureteric stones >8mm
Criteria for Inpatient Admission
The majority of renal stones can be treated in the outpatient setting. However, criteria that often warrant the need for hospital admission include:
- Post-obstructive acute kidney injury
- Uncontrollable pain from simple analgesics
- Evidence of an infected stone(s)
- Large stones (>5mm)
Stent Insertion or Nephrostomy
Patients with any evidence of obstructing stones may warrant primary ureteroscopy or ESWL (see below) to clear the stone, but if they have any evidence of infection or acute kidney injury, they need urgent decompression with stent insertion or a nephrostomy.
Retrograde stent insertion is the placement of a stent within the ureter, approaching from distal to proximal via cystoscopy (Fig. 4). It allows the ureter to be kept patent and temporarily relieve the obstruction.
A nephrostomy is a tube placed directly into the renal pelvis and collecting system, relieving the obstruction proximally (Fig. 5). If required, an anterograde stent can subsequently be passed via the same tract made.
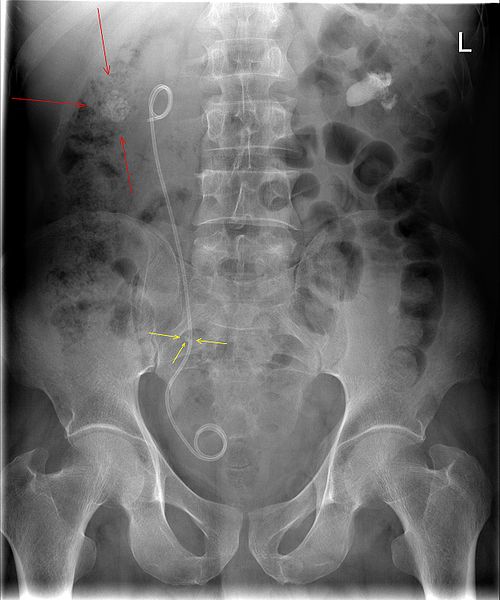
Figure 4 – AXR showing a JJ stent inserted, with associated right renal stone
Definitive Management
Definitive treatment of retained renal or ureteric stones can be achieved by several methods for stones that do not pass spontaneously.
Extracorporeal Shock Wave Lithotripsy (ESWL) involves targeted sonic waves to break up the stone, to then be passes spontaneously. This is typically reserved for small stones (<2cm), performed via radiological guidance (either X-ray or ultrasound imaging). Contra-indications include pregnancy and those on anticoagluants or coagulopathy
Percutaneous nephrolithotomy (PCNL) is used for renal stones only, being the preferred method for large renal stones (including staghorn calculi). Percutaneous access to the kidney is performed, with a nephroscope passed into the renal pelvis. The stones can then be fragmented using various forms of lithotripsy.
Flexible uretero-renoscopy (URS) involves passing a scope retrograde up into the ureter, allowing stones to be fragmented through laser lithotripsy and the fragments subsequently removed.
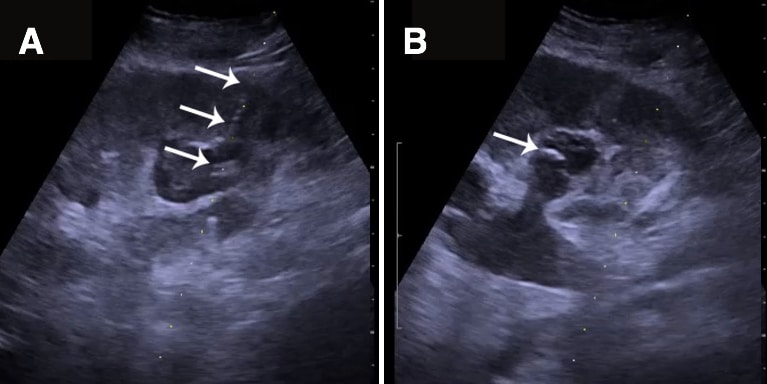
Figure 5 – Percutaneous nephrostomy tube placed through a calyx into the lower pole of a kidney with hydronephrosis; the tube in (A) and the curled distal end (the “pigtail”) in (B)
Complications
The main complications that can occur from ureteric stones is infection and post-renal acute kidney injury, however both can be treated if managed early.
Recurrent renal stones can lead to renal scarring and loss of kidney function
Management of Recurrent Stone Formers
Patients who are recurrent stone formers often need specialised management, with the underlying cause identified and managed as appropriate.
All these patients should be advised to stay hydrated. If the patient is unable to retrieve any passed stones, ensure serum urate and calcium levels are checked.
Specific management options depend on the underlying stone composition:
- Oxalate stone formers should be advised to avoid high purine foods and high oxalate foods (such as nuts, rhubarb, and sesame)
- Calcium stone formers should have PTH levels checked to exclude any primary hyperparathyroidism and avoid excess salt in their diet
- Urate stone formers should be advised to avoid high purine foods (such as red meat and shellfish) and may need to be considered for urate-lowering medication (e.g. allopurinol)
- Cystine stone formers may warrant genetic testing for underlying familial disease
Bladder Stones
Bladder stones typically form from urine stasis within the bladder, hence are commonly seen in cases of chronic urinary retention. They may also occur secondary to infections (classically schistosomiasis) or as passed ureteric stones, however if they are identified in a male patient, then bladder outflow surgery should be considered.
They will most often present with lower urinary tract symptoms and require investigation the same as for renal and ureteric stones. Definitive management is through cystoscopy, allowing the stones to drain or fragmenting them through lithotripsy if required.
The chronic irritation of the bladder epithelium from a bladder stone can also predispose to the development of SCC bladder cancer.
Key Points
- Renal stones are common, with several subtypes of composition possible
- Patients classically present with one-sided colicky flank pain, radiating to the groin
- Gold standard for diagnosis is a non-contrast CT KUB scan
- Most stones will pass naturally with analgesia and hydration, however several management options are available for those that remain


