Introduction
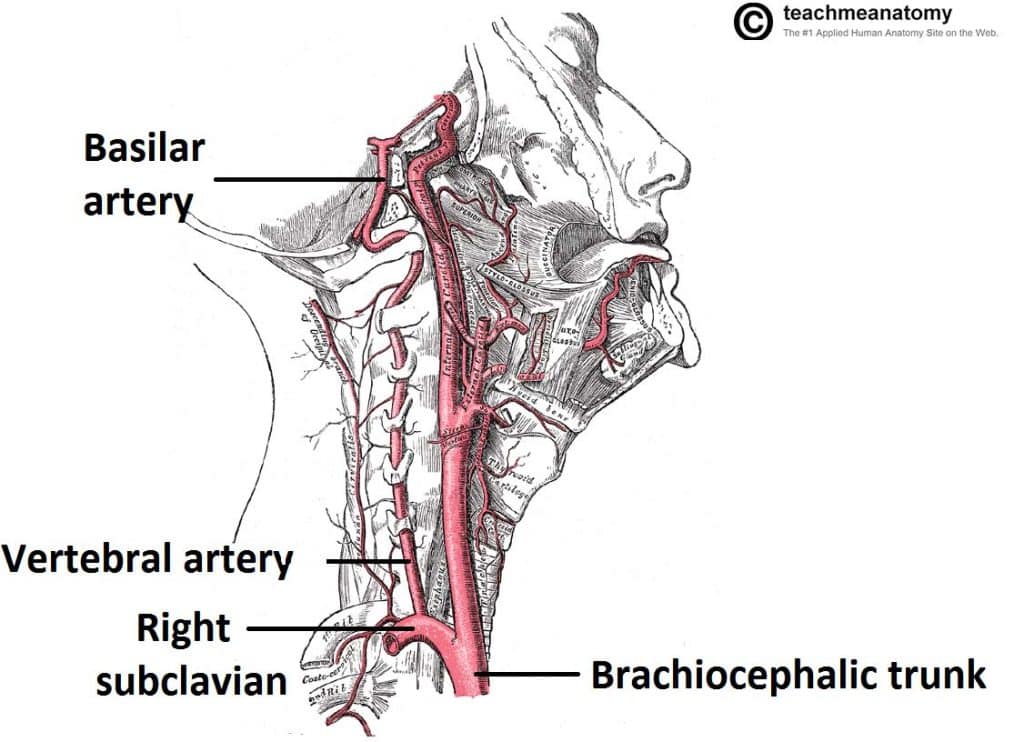
Subclavian steal syndrome is a rare condition causing syncope or neurological deficits when the blood supply to the affected arm is increased through exercise. Subclavian steal is secondary to a proximal stenosing lesion or occlusion in the subclavian artery, typically on the left.
In order to compensate for the increased oxygen demand in the arm, blood is drawn from the collateral circulation, which results in reversed blood flow in the ipsilateral vertebral artery (or less commonly the internal thoracic artery).
The syndrome comprises of both cerebral and upper limb clinical features. The condition is twice as prevalent in males and occurs three times more often on the left side compared to the right*.
Stenosis in the subclavian artery is commonly caused by atherosclerosis, however less common causes of the condition include vasculitis, thoracic outlet syndrome (e.g. cervical rib), or complications following aortic coarctation repair
*Interestingly, 1 out of every 50 people have their vertebral artery arising directly from the aortic arch, thereby avoiding any chance of the syndrome developing.
Coronary-Subclavian Steal Syndrome
Coronary-Subclavian Steal Syndrome occurs in patients who have undergone an Internal Mammary Artery (IMA) Graft. An increase in oxygen demand in the left arm then steals blood from the IMA leading to cardiac ischaemia.
Clinical Features
In periods of arm activity, reversal of the blood supply to the posterior cerebral circulation via the vertebral artery can result in a wide range of cerebral symptoms, including vertigo, diplopia, dysphagia, dysarthria, visual loss, or syncope.
Patients may also present with arm claudication due to the occluding lesions, such as arm pain or paraesthesia, made worse with arm movement.
Investigations
Suspected cases should initially be investigated with duplex US scan, which can show the retrograde flow in the affected vertebral artery during exercise. Routine chest radiograph can aid in assessing for any external compression on the subclavian artery.
Definitive investigation is via CT angiography (Fig. 2) or MR angiography, which will identify the anatomy of the occlusive lesion in the arm and can also help to assess the cerebral vasculature*
*80% of patients with subclavian steal syndrome will also have additional vascular disease in the rest of the cerebral circulation

Figure 2 – CT angiogram of aortic arch, demonstrating a stenosis of the left subclavian artery (red circle) with reduced blood flow distally (purple arrow) and no contrast visible in vertebral artery
Disease Severity Risk Scoring
Risk scoring of subclavian steal syndrome can be classified into three grades:
- Pre-Subclavian Steal – demonstrating purely a reduced anterograde vertebral flow
- Intermittent Alternating Flow – antegrade flow occurs in the diastolic phase and retrograde flow occurs in the systolic phase
- Advanced Disease – there is a permanent retrograde flow
Management
Conservative Management
All patients should be started on anti-platelet and statin therapy, if suitable.
Patients should have any modifiable cardiovascular risk factors addressed, such as smoking cessation, weight loss, and optimising diabetic control.
Surgical Management
Occlusions may be treated either through endovascular or bypass techniques, although these have risks of stroke and damage to the brachial plexus.
Use of percutaneous angioplasty ± stenting (Fig. 3) has reported success rates upwards of 90%, albeit with higher rate of restenosis with worsening disease severity.
Use of bypass should be considered for longer or distal occlusions; options include carotid-subclavian bypass (5 year patency rates reported at 80%) or axillo-axillary bypass.
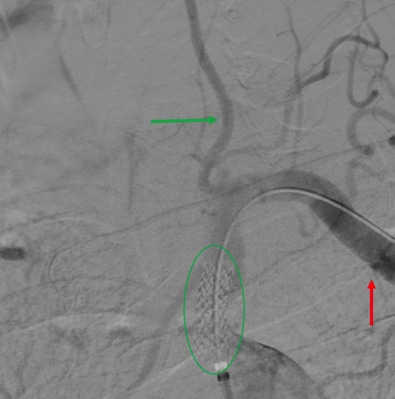
Figure 3 – Angiogram of aortic arch, showing a left subclavian artery stent placed (circle) with distal blood flow (red arrow) and contrast extending into left vertebral artery (green arrow)
Key Points
- Subclavian steal syndrome occurs secondary to a proximal stenosing lesion or occlusion in the subclavian artery
- Blood is drawn from the collateral circulation, which results in reversed blood flow in the ipsilateral vertebral artery
- Patients can present with limb claudication and / or cerebral symptoms
- Mainstay of investigation is through angiography
- Patients should have cardiovascular risk factors appropriately managed, with the occlusion treated surgically through endovascular or bypass techniques