Introduction
Urethritis is the inflammation of the urethra, most often due to infection. The infection can be classified by its aetiology, either as gonococcal urethritis and non-gonococcal urethritis.
Gonococcal urethritis is caused by N. gonorrhoeae, whereas non-gonococcal urethritis is caused most commonly by C. trachomatis, followed by M. genitalium, and T. vagninalis.
Risk Factors
The main risk factors for the condition are age <25yrs, men who have sex with men, previous sexually transmitted infection (STI), recent new sexual partner, or more than one partner in the last year.
Clinical Features
The typical presenting symptoms of urethritis are dysuria, penile irritation, and discharge from the urethral meatus.
Eliciting a thorough sexual history can help narrow down the likely pathogens and risk stratify the burden of disease, as well as inform necessary additional sexual health screens and partner notification.
Patients can also present with features from the complications of urethritis, such as epididymitis or reactive arthritis (see below).
Reactive Arthritis
Reactive Arthritis is a sterile inflammatory arthritis caused by a distant infection producing an autoimmune response to certain joints. Commonly caused by Chlamydia trachomatis, Chlamydia pneumoniae, Campylobacter spp., Shigella spp., or Salmonella spp..
It normally presents as an oligoarthritis, typically in the lower limb joints, alongside potential other extra-articular manifestations including conjunctivitis or uveitis, urethritis, cervicitis, or prostatitis, keratoderma blenorrhagicum or painless oral ulcers, or malaise or fatigue.
Around 80% of reactive arthritides resolve within 6 months. Treatment involves rest and treating the affected joint(s) with NSAIDs or local steroid injections; treatment of underlying condition often has limited impact on overall disease progression.
Differential Diagnosis
The main differential is balanitis, which is inflammation of the glans penis. This presents with pruritis, erythema, and discharge between the foreskin and the glans, contrasting with the urethral discharge and dysuria of urethritis. Balanitis is more common in older patients and can be secondary to bacterial or fungal infection.
Investigations
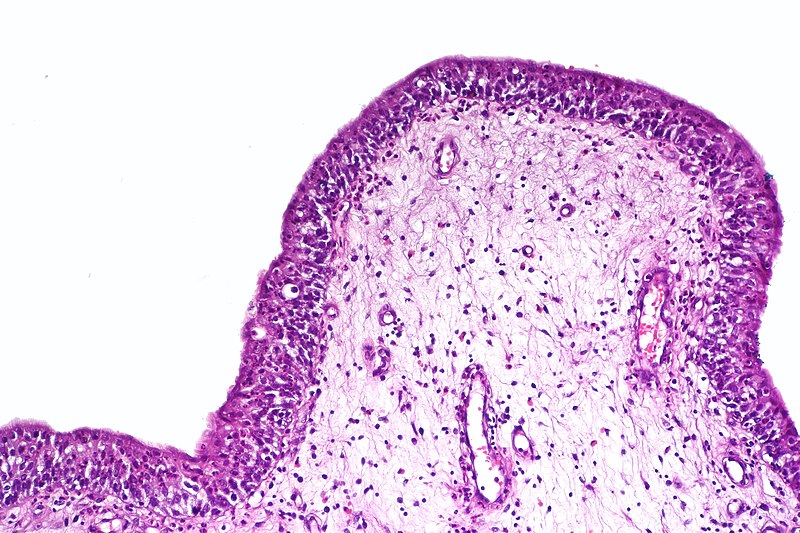
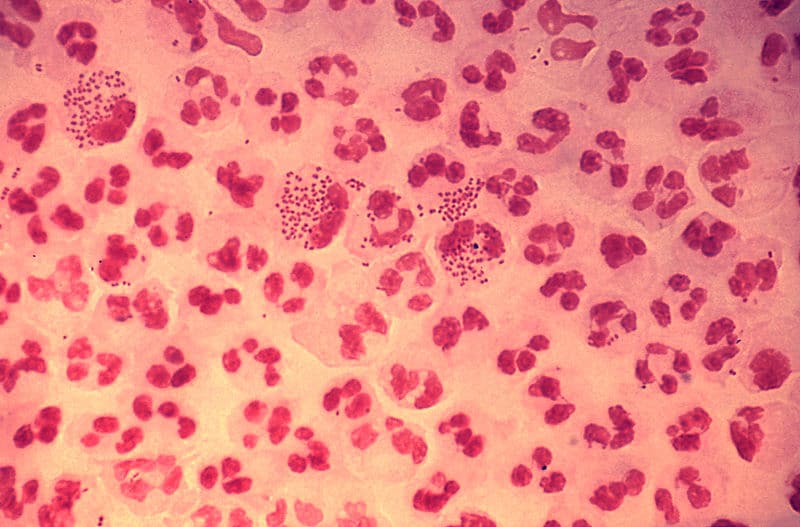
Urethral gram stain under microscopy should be performed on urethral swabs if available (available in the GUM setting); pus cells suggest urethritis, and any presence of Gram negative diplococci are highly sensitive for a gonococcal infection.
Gold standard diagnosis is from a first-void urine being sent for Nucleic Acid Amplification Test (NAAT), for N. gonorrhoeae, C. trachomatis, and M. genitalium.
All suspected cases should also have a mid-stream urine dipstick performed, with a low threshold for sending for culture (MC&S). Triple site testing for culture should also be done in the case of gonococcal infection.
Consider further STI screening, such as HIV and syphilis serology, as appropriate. Semen culture can also be appropriate where prostatitis is a suspected.
Management
Initial Management
Antibiotic management is the mainstay of initial management, with the specific regime dependent on the underlying or suspected causative organism.
Current BASHH guidelines recommend:
- Gonococcal = Ceftriaxone 1g IM single dose + Azithromycin 1g PO single dose
- Non-gonococcal = Doxycycline 100mg PO BD for 7 days OR Azithromycin 1g PO single dose*
*If trichomonas spp. are seen on microscopy, consider Metronidazole 2g PO single dose; in cases of recurrent NGU other regimens are also considered, such as azithromycin 500mg PO stat and 250mg for 2 days or moxifloxacin 400mg PO OD for 10-14 days
Mycoplasma genitalium is a growing concern as an under-treated cause of recurrent non-gonococcal urethritis and increasingly it will be relevant to run resistant tests in the cases of M. genitalium infections.
Long-term Management
Patients should abstain from sexual activity for 7 days after antibiotic course is finished, symptoms have resolved, and their sexual partners have been treated. In cases of gonorrhoea, a test of cure is required.
Counsel patients on condom use and advise the patient to notify their sexual partners to attend the sexual health clinic for testing and treatment.
Contact Tracing
Guidelines from the Royal College of General Practitioners and RCGP and the British Association for Sexual Health and HIV (BASHH) advise the following
|
At time of diagnosis? |
Gonorrhoea | Chlamydia |
Non-specific urethritis |
| Symptomatic | All sexual partners in previous 2 weeks | All sexual partners in previous 4 weeks | All sexual partners in previous 4 weeks |
| Non-symptomatic | All sexual partners in previous 3 months | All sexual partners in previous 6 months | All sexual partners in previous 4 weeks |
Key Points
- Urethritis is the inflammation of the urethra, most often due to infection
- It can be classified by its aetiology into either gonococcal urethritis and non-gonococcal urethritis
- Patients present with dysuria, penile irritation, and discharge
- Antibiotic management is the mainstay of initial management, however need to ensure appropriate advice given and contact tracing performed