Introduction
Cholangiocarcinoma is a malignancy of the biliary system. It can occur at any site along the biliary tree, although predominantly arises in the extrahepatic biliary system; incidence of intrahepatic cholangiocarcinoma is increasing for unknown reasons.
The incidence is 1-2 per 100,000 population per year in many high-income setting, with over two-thirds of these cases in patients >65yrs. There is a higher incidence in South-East Asia due to the association with chronic endemic parasitic infections from liver flukes, as well as the likely contribution of chronic hepatitis C infection.
Histologically, 95% of bile duct cancers are adenocarcinomas, arising from cholangiocytes within the biliary tree with squamous cell carcinomas and other rarer types of bile duct cancers include sarcomas, lymphomas, and small cell cancers seen.
Klatskin Tumours
The most common site for bile duct cancers is at the bifurcation of the right and left hepatic ducts, termed Klatskin tumours or hilar cholangiocarcinoma, and account for 60% of cholangiocarcinoma.
These tumours generally invade local structures, such as the portal vein and hepatic arteries, and metastasise to local lymph nodes, before spreading to the peritoneal cavity, lung, and liver.
In this article, we shall look at the risk factors, clinical features and management of a patient with cholangiocarcinoma.
Risk Factors
The main risk factors for cholangiocarcinoma include:
- Primary sclerosing cholangitis (lifetime risk of 10-20%)
- More likely to have multifocal disease
- Congenital (Caroli’s disease, choledochal cyst)
- Intraductal gallstone formation
- Infective (Liver flukes, hepatitis virus)
- Toxins (Chemicals in rubber and aircraft industry)
- Liver cirrhosis
Clinical Features
Intrahepatic cholangiocarcinoma is generally asymptomatic until a late stage in the disease, whereas extrahepatic cholangiocarcinoma will typically present early.
Patients will present with jaundice, along with associated pruritus, steatorrhoea, non-specific abdominal pain, or dark urine. In advanced disease, weight loss and lethargy can occur.
On examination, jaundice and cachexia are often evident. Courvoisier’s law can be applied in clinical assessment.
Courvoisier’s Law
Courvoisier’s law states that in the presence of jaundice and an enlarged or palpable gallbladder, malignancy of the biliary tree or pancreas should be strongly suspected as the cause is unlikely to be gallstones.
Investigations
Biochemical investigations will confirm an obstructive jaundice (elevated bilirubin, ALP, and ɣGT). The tumour markers CEA and CA19-9 may also be elevated, but are non-specific and generally less useful in diagnosis. The mainstay of diagnosis comes from radiology*.
*Ultrasound scanning may initially show dilated biliary ducts and on occasion can demonstrate tumour location within the biliary tree, however is highly user dependent and CT or MRI imaging are generally required for diagnosis
Radiological Investigations
Magnetic resonance cholangiopancreatography (MRCP) is the gold standard imaging modality* for the diagnosis of cholangiocarcinoma, as it affords improved analysis of tumour location and biliary obstruction as well as vascular involvement, lymph node spread and metastasis within the liver parenchyma.
The use of CT imaging can assess for tumour location and any evidence of arterial or venous invasion, especially when contrast enhancement is used. Longstanding tumours with biliary obstruction may also cause segmental atrophy, which can be assessed on CT scan.
Endoscopic retrograde cholangiopancreatography (ERCP) or Percutaneous Transhepatic Cholangiography (PTC) may be required to allow biliary decompression and can be used to obtain tissue brushings for cytological diagnosis. Direct visualisation of the bile duct by endoscopic cholangioscopy may assist in diagnosis of indeterminate lesions, by allowing biopsies to be taken for histological diagnosis.
*Cholangiocarcinoma is characterised by hyperintensity on T2-weighted MRI with slow delayed enhancement after contrats administration
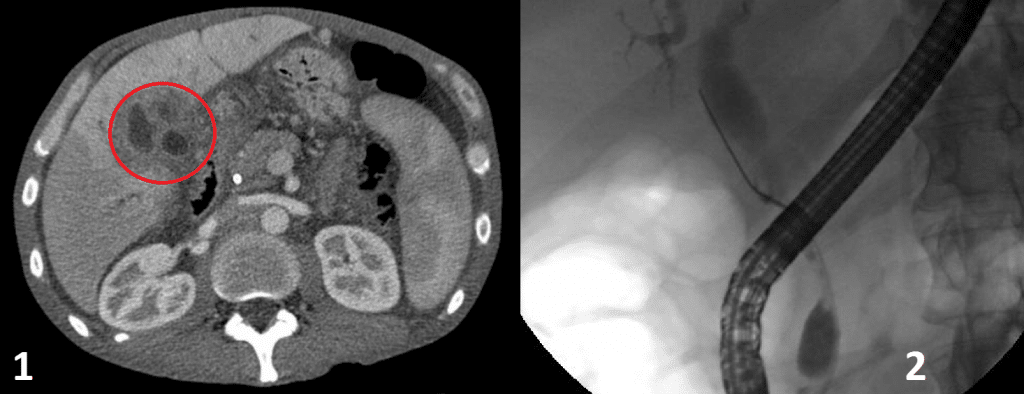
Figure 2 – Imaging for Cholangiocarcinoma. (1) CT scan showing cholangiocarcinoma (circled) (2) ERCP showing common bile duct stricture and dilatation of the proximal duct
Staging of the disease is best done via a combination of contrast-enhanced triple phase CT imaging and contrast-enhanced MRI of the liver. Staging for cholangiocarcinoma is classified by TNM staging as for most cancers, with seperate T-stage classification for intrahepatic and hilar cholangiocarcinoma respectively.
Management
The definitive cure for cholangiocarcinoma is complete surgical resection. However, the majority of patients have inoperable disease at the time of presentation, due to bilobar disease, vascular involvement, distant metastasis, or patient frailty. Only 10-15% of patients are suitable for surgical intervention and approximately 50% have recurrence after surgery within 5 years.
Intrahepatic or Klatskin tumours require a partial hepatectomy and reconstruction of the biliary tree. In hilar cholangiocarcinoma, remant liver volume may be low and preoperative procedures, such as portal vein embolisation, may be needed to increase the liver volume. Patients with distal common duct tumours require a pancreaticoduodenectomy (either a Whipple’s procedure or a Pylorus preserving pancreaticduodenectomy (PPPD)).
Both chemotherapy and radiotherapy may be used in some cases as adjuvant treatments after surgery. Recent data has shown there is a significant survival benefit with adjuvant capecitabine chemotherapy after surgical resection, whilst radiotherapy after R1 resection may also have benefit.
Palliative
Most cases will end up only having palliative management. The palliative treatment options in cholangiocarcinoma include:
- Stenting – ERCP and PTC may be used to stent the biliary tree and relieve obstructive symptoms
- Surgery – Surgical bypass procedures by formation of hepaticojejunostomy may be required if the obstruction cannot be relieved by stenting
- Medical – Palliative radiotherapy or chemotherapy options can be discussed with the patient
Prognosis
Long term survival is generally poor and treatment should be aimed at good symptom relief and palliative management. The average survival is 12-18 months from diagnosis, as most patients have unresectable disease at the time of presentation.
In patients undergoing aggressive surgery, 5 year survival rates are 10-40%. Survival appears to be better for distal tumours, at up to 54% at 5 years.
Key Points
- Cholangiocarcinoma is a relatively rare malignancy, 95% of which are adenocarcinomas
- Patients will present often in late-stage disease, commonly with obstructive jaundice
- The gold-standard investigation is MRCP +/- ERCP or PTC for relief of biliary obstruction and to provide tissue diagnosis
- Definitive cure for cholangiocarcinoma is complete surgical resection, however most patients will only be suitable for palliative management