Introduction
Burn injuries can have wide-ranging physical and psychological sequelae, with many patients requiring treatment in specialised centres. In the UK, 175,000 patients present to Emergency Departments with a burn each year.
Whilst most burns are minor, major burns will require close monitoring and management, especially to those of increasing age or with extensive co-morbidities.
The classification of burns injury is summarised in the table below:
| Type | Description | |
| Thermal | Scald | Injury caused by hot liquids and steam, common in children and older patients |
| Flame | Direct exposure to fire, can be associated with concomitant inhalation injury | |
| Flash | Indirect exposure to flame | |
| Contact | Direct contact with an extremely hot or cold object | |
| Chemical | Acid | Results in denaturation of protein in tissue and resultant coagulation necrosis |
| Alkali | Results in denaturation of protein in tissue and resultant liquefaction necrosis* | |
| Electrical | Direct contact | Current from an electrical source passes directly through the body†, resulting in an entry and exit wound and can cause significant internal damage to deeper structures |
| Electrical arc | A flash thermal burn occurs due to an electrical arc coming briefly into contact with skin, results n thermal burns mainly | |
Table 1 – Classification of burns injury; *Alkaline buns often result in deeper and more severe burns, due to protein denaturation and fat saponification; †Complications of electrical burns include compa ramens syndrome, cardiac arrhythmias, and rhabdomyolysis
Inhalation Injury
An inhalation injury is damage to the airway, secondary to the inhalation of hot air or noxious gases. Inhalation injury should be suspected whenever an injury is from a flame or smoke exposure in enclosed environment. Mortality in burns increases by 20% when associated with an inhalation injury.
Anyone with features of airway compromise, such as stridor, hoarse voice, or respiratory compromise, post-injury will likely need a definitive airway placed (i.e. intubation). More subtle features to suggest a potential airway injury include singed nasal hairs, facial burns, or soot deposits around the nose.
Burn Initial Management
When assessing a patient with burns injury, a thorough A to E assessment is vital. Once performed and the patient stable, try to elicit details regarding the mechanism of the burn, as it can provide clues to the likely depth, associated inhalation injury, and concomitant traumatic injuries
A major burn is any burn with >15% TBSA (>10% in children) of partial or full-thickness burns (i.e. not including superficial burns). Major burns can result in profound inflammatory responses and large fluid shifts occurring, and aggressive fluid resuscitation is often required to mitigate burn shock.
Ensure any source of burning is removed as a priority, as is any non-adherent clothing.
Initial Assessment
The initial assessment of a patient with a burns injury requires an A to E assessment (discussed more here), however there are a few specific points to be aware of for burns patients:
- Airway – Evaluate for signs of inhalation injury; pre-emptive intubation may be required if suspected or high-risk. Remember to protect cervical spine until clinically cleared
- Breathing – Administer 100% oxygen via non-rebreather reservoir mask. In more extensive burns, evaluate the need for escharotomy, especially if circumferential chest burns are present. Obtain an ABG and check carboxyhaemoglobin levels (for carbon monoxide poisoning)
- Circulation – Site two wide bore intravenous cannula (avoiding insertion through burned tissue, if possible) and take routine bloods, including group and screen, clotting, and creatinine kinase. Aggressive intravenous fluid therapy is indicated (discussed later) and insertion of a urinary catheter is essential for fluid balance monitoring
- Disability – Evaluate neurological status using the Glasgow Coma Scale and ensure to check the temperature, as there is an increased risk of hypothermia
- Exposure – The patient should be fully exposed to get an accurate estimation of the percentage of total body surface area (%TBSA) burned and to check for any concomitant injuries*. Ensure the patient is given a tetanus booster if their status is uncertain.
*Remember that electrical burns may show only a small area of external injury, but have caused significant visceral injury
Intravenous morphine should be used where required for analgesia. Ensure an ECG and CXR are performed, and start a strict fluid balance chart.
Wound dressing protocols vary, however in general, if the patient is to be transferred to higher-level burn care, initially dress the wound with Cling film to allow full evaluation of burn depth, whilst minimising fluid losses from the affected wounds.
Hypothermia is a severe risk following burns injury, due to the extensive heat and fluid loss that can occur from the burns sites. As such, assessment in a warmed room, giving warmed fluids if possible, and reducing wound exposure time can all help in limiting hypothermia.
Minor Burns
Rapid and thorough first aid should be performed for all minor burns. General management principles for the management of minor burns starts with removing the source of the burn.
Any non-adherent clothing should be removed, before the wound is cooled under running water for twenty minutes as soon as possible, as this promotes re-epithelialisation.
Assessing Burn Severity
The severity of a burn is generally defined by the percentage total body surface area (%TBSA) burned and burn depth.
Accurate estimation of %TBSA burned is a critical step in guiding appropriate burns management as it determines the initial fluid volume requirements for resuscitation, and whether or not the patient should be considered for transfer to specialist care.
Various techniques can be used to estimate %TBSA, such as Wallace’s Rule of Nines (Fig. 1A), the “Rule of Palm” where the patients palm area represents 1% of their TBSA, or a Lund & Browder Chart (Fig. 1B) which are most used in paediatric cases.
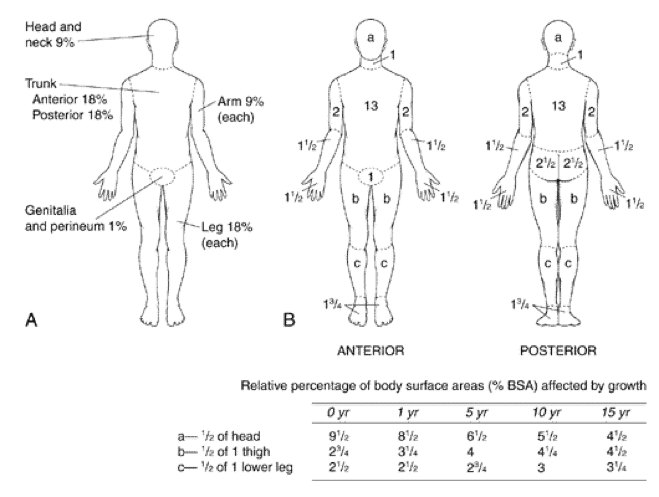
Figure 1 – (A) Wallace’s Rule of Nines (B) Lund & Browder Chart
Assessing Burn Depth
Burn depth approximation is important as it guides therapy (Table 2). More superficial burns may heal spontaneously (albeit are often more painful), while deeper burns may require further intervention (Fig. 2); deeper burns also carry an increased risk of complications.
Burn depth does not, however, guide initial resuscitative efforts and so administration of adequate fluid resuscitation should not be delayed in favour of accurate burn depth evaluation.
|
Burn Thickness |
Deepest Layer Involved |
Appearance |
Pain |
Prognosis |
| Superficial | Epidermis | Dry, blanching, erythema | Painful | Heals without scarring, 5-10days |
| Superficial partial-thickness | Upper dermis | Blisters, wet, blanching, erythema | Painful | Heals without scarring, <3 weeks |
| Deep partial-thickness | Lower dermis | Yellow or white, dry, non-blanching | Decreased sensation | Heals in 3-8 weeks, likely to scar if healing >3 weeks |
| Full thickness | Subcutaneous tissue | Leathery or waxy white, non-blanching, dry | Painless | Heals by contracture >8 weeks, will scar |
Table 2 – Classification of Burns by Depth
Fluid Resuscitation
Fluid resuscitation following burn injury allows for adequate intravascular volume to limit hypovolaemia, maintain organ perfusion, and minimise tissue ischaemia in the immediate post-burn period.
Fluids are calculated from the time of the burn, not the patient’s hospital arrival time. If the patient is clinically shocked on arrival, this should be corrected prior to calculating any burn fluid requirements.
The modified Parkland formula is the one most commonly used for directing initial fluid requirements. This purely acts as a guide, as every patient should be monitored closely and reassessed regularly to gauge their response to the administered fluid.
The modified Parkland formula provides a guide for the volume of crystalloid fluid (ideally Hartmanns solution) to be administered in the first 24 hours post-burn:
- Adults:
- 3mL x Weight (kg) x % TBSA burn
- Children:
- 3mL x Weight (kg) x % TBSA burn
- PLUS Maintenance fluids (0.5% glucose in 0.45% saline)
50% of the calculated volume is given within the first 8 hours post-burn, and the remaining 50% is given in the remaining 16 hours.
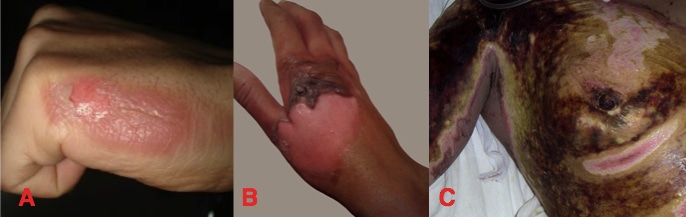
Figure 2 – Types of Burn (A) Superficial (B) Partial (C) Deep
Goal-Directed Therapy
The goal of fluid resuscitation is achieving adequate end-organ perfusion. Due to the systemic inflammation seen in burns patients, conventional markers of fluid balance are not always feasible.
Urine output can be monitored closely as the main marker of fluid balance status, which should be maintained (in adults) at >0.5mL/kg/hr (children 1ml/kg/hr). Other measures include use of mean arterial pressures (MAPs) and blood gas measurements.
Ongoing Care
Depending on the injuries involved, patients with burns may require transfer to either a burns unit or a burns centre (see Appendix):
- Burn Units are facilities that have a specialised burns ward staffed by skilled burns professionals, capable of caring for moderate level of injury complexity.
- Burn Centres represent the highest level of inpatient burn care, with immediate operating theatre access and highly-skilled critical care staff, for the management of highly complex burn injuries.
Complications of burns injuries include airway compromise and respiratory failure, fluid loss and electrolyte imbalance, hypothermia, and compartment syndrome.
Key Points
- As with all unwell patients, ensure a rapid and thorough physiological assessment and management using a structured A to E approach
- Ensure adequate warming and fluid resuscitation is provided, due to extensive fluid and heat losses that can occur
- Calculate the degree and extent of the burns, as this will influence need for clinical transfer
- Complications of burns injuries include airway compromise and respiratory failure, fluid loss and electrolyte imbalances, hypothermia, and compartment syndrome
Appendix
|
Criteria |
Burns Unit |
Burns Centre |
| %TBSA | 10-39% | ≥40%, or ≥25% with inhalation injury |
| Depth | Deep partial or full-thickness | |
| Site | Specialised areas (hands, feet, face, perineum, genitals, over major joint) | |
| Non-blanching circumferential burns | ||
| Aetiology | Any chemical, electrical, friction, or cold injury require discussion with burns specialists. | |
| Other | Suspected non-accidental injury (NAI) | Concomitant major trauma with burn injury meeting centre threshold |
| Pregnant patients | Concomitant severe co-morbidities and patients >65yrs with ≥25% TBSA burns | |
| Concomitant trauma with burn injury |
Table 3 – Suggested Criteria for Determining the Transfer to Burns Unit versus Transfer to Burns Centre
