A blood product is any part of the blood that is collected from a donor for use in a blood transfusion. Although prescribing blood products may feel much the same as prescribing any other fluid, it is a decision that should be taken seriously, for a number of reasons:
- Transfusion reactions are relatively common, even in those with appropriately cross-matched blood.
- Blood products are scarce and should therefore only be used when necessary.
- Blood group incompatibility is a rare but life-threatening complication. Blood products therefore need to be appropriately cross-matched and checked to avoid severe consequences.
Current NICE guidelines recommend a restrictive haemoglobin concentration threshold of 70 g/L for those who need red blood cell transfusions (without any major haemorrhage or acute coronary syndrome) and a haemoglobin concentration target of 70-90 g/L after transfusion
In this article, we shall look at blood groups, the different types of blood products, and their administration.
Blood Grouping
To minimise the risk of transfusion reactions, the blood group of the donor and recipient must be considered. In blood transfusions, there are two important blood groups, the ABO blood system and the group D of the rhesus system.
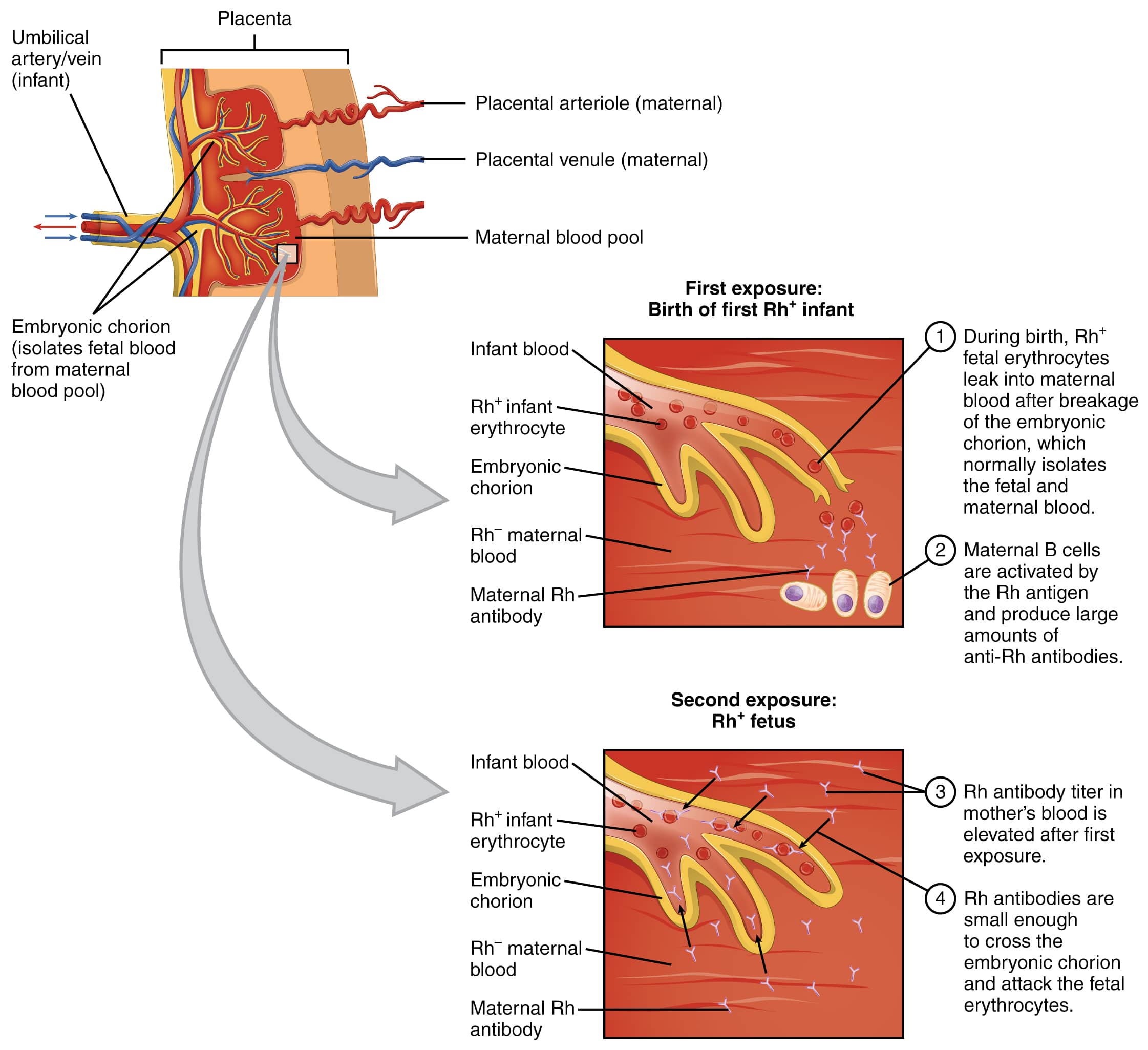
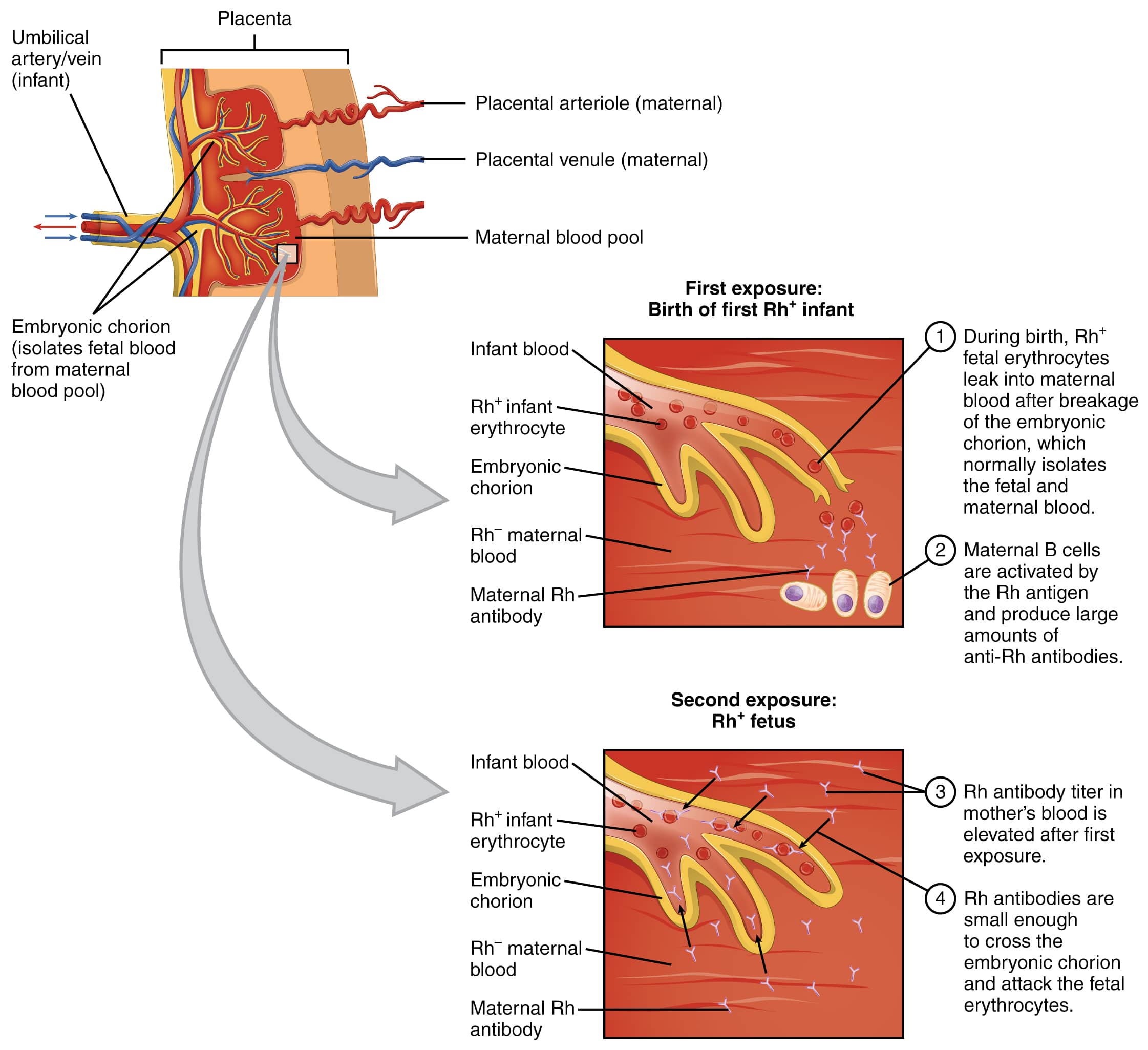
Rhesus D (RhD) Group
A patient’s blood group can initially be classified as ‘RhD+’ or ‘RhD-‘: this refers the presence or absence of Rhesus D surface antigens on the red blood cells (RBC). Approximately 85% of the population is RhD+ (they have RhD antigens present) and 15% are RhD– (RhD antigens are absent).
A RhD- patient will make RhD antibody if they are given RhD+ blood. Clearly, this will not matter for the patient; a RhD- patient, who is given RhD+ blood, and therefore makes anti-D, cannot then go on to attack their own red blood cells as they do not have RhD present on their RBC membrane.
However, this does cause potential problems during pregnancy as anti-D antibodies can cross the placenta, such as may occur in the following example:
- A woman is born with RhD- blood. Her partner is RhD+ and she becomes pregnant with a fetus that is also RhD+. During childbirth, she comes into contact with the foetal (Rh+ve) blood and develops antibodies to it.
- She later becomes pregnant with a second child that is also Rh +ve.
- The woman’s anti-D antibodies cross the placenta during this pregnancy and enter the foetal circulation, which contains RhD+ blood, and bind to the foetus’ RhD antigens on its RBC surface membranes.
- This causes the foetal immune system to attack and destroy its own RBCs, leading to foetal anaemia. This is termed haemolytic disease of the newborn (HDN).
We therefore give RhD specific blood to women in order to avoid HDN. In men, this is clearly not a concern so, although it is preferable to give correctly cross-matched blood, it is possible to give a RhD- male some RhD+ blood if that is all that is available in an emergency setting.
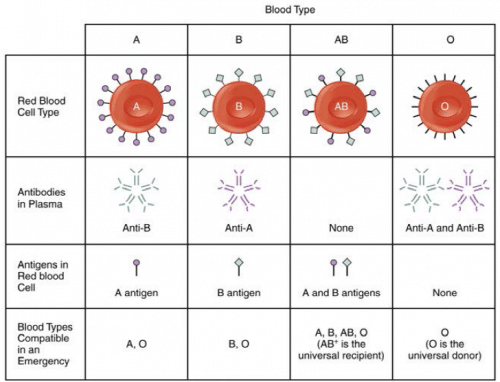
ABO Group
The ABO blood group refers to the presence of A and / or B antigens on the surface of red blood cells. The specific ABO group is important for all individuals undergoing a potential blood transfusion. In the simplest terms, you produce antibodies to bind to the surface antigens (A or B) that are not present on your own red blood cell surface membrane. As a consequence, a few key terms are important to understand:
- Universal donor: O-ve – this blood can be given to anybody, irrespective of the recipient’s blood group, because there are no AB or Rhesus antigens on the donor RBC surface membrane. The recipient can have both A, B and Rhesus antibodies in their circulation, but they will likely not reject this donor blood, as there are no ABO or Rh antigens to attack.
- Universal Acceptor: AB+ve – you can give this recipient any donor blood, irrespective of the ABO or Rhesus status. The recipient does not have any A, B, or Rhesus antibodies in their circulation and therefore cannot mount an immune response to the donor blood.
Blood Tests
There are two blood tests that can be performed prior to blood transfusion, the group and save and the cross-match:
- Group and Save (G&S) – determines the patient’s blood group (ABO and RhD) and screens the blood for any atypical antibodies. The process takes around 40 minutes and no blood is issued. A G&S is recommended if blood loss is not anticipated, but blood may be required should there be greater blood loss than expected.
- Crossmatch (X-match) – involves physically mixing the patient’s blood with the donor’s blood, in order to see if any immune reaction takes places. If it does not, the donor blood is issued and can be transfused in to the patient. This process also takes ~40 minutes, in addition to the 40 minutes required to G&S the blood (which must be done first). A X-match is done if blood loss is anticipated, but the surgeon will usually inform you of this.
Requesting Blood Products
At every stage of requesting blood products, strict adherence to the procedures in place is required to prevent the patient being given incorrect blood, including:
- Using 3 points of identificationto check you are with the correct patient (name, Date of Birth (DOB), and patient number).
- Consent the patient appropriately – many transfusion request forms will now have a script on them, which you should read to the patient. A consent form (as you would use for consent for any procedure) is completed.
- Labeling the bottle at the bedside (pre-printed stickers for blood transfusion are usually not allowed in many countries, including the UK)
- Completing the transfusion request form at the bedside. Before you put the blood bottle into the request bag, check with the patient that they are happy you have labelled things correctly.
CMV-Negative Blood Products
Cytomegalovirus is a common congenital infection that may lead to sensorineural deafness and cerebral palsy. Consequently, CMV negative blood should be given to women during pregnancy, intra-uterine transfusions, and to neonates (up to 28 days).
Irradiated Blood Products
Irradiated products are required to reduce the risk of graft-versus-host-disease in at risk populations. The following groups should receive irradiated blood:
- Those receiving blood from first or second-degree family members
- Patients with Hodgkin’s Lymphoma
- Recent haematpoietic stem cell(HSC) transplants
- After Anti-Thymocyte Globulin (ATG) or Alemtuzumab therapy
- Those receiving purine analogues (e.g. fludarabine) as chemotherapy
- Intra-uterine transfusions
Administering Blood Products
If a patient requires more than one unit of blood, each unit must be prescribed individually. Whilst the patient is receiving the transfusion, there are specific observations timings that should be carried out:
- Before the transfusion starts.
- 15-20 minutes after it has started.
- At 1 hour.
- At completion.
Blood products should only be administered through a green (18G) or grey (16G) cannula, otherwise the cells haemolyse due to sheering forces in the narrow tube.
NICE guidelines suggest single unit red blood cell transfusions for the surgical patient who does not have active bleeding, reassessing the patient after each transfusion
Types of Blood Products
When blood is harvested from donors, it is separated into its constituent parts.
Remember to ensure that all of the above products are administered through a blood giving set rather than a normal fluid giving set. A blood giving set contains a filter in the chamber, whereas a normal fluid giving set does not.
Packed Red Cells
- Major constituents– Red blood cells
- Indications– (i) Acute blood loss; (ii) Chronic anaemia, where the Hb ≤70g/L (or ≤100g/L in those with cardiovascular disease) or symptomatic anaemia
- Duration over which it is administered –2-4 hours. It must be completed within 4 hours of coming out of the store
1 unit of blood should increase a patient’s haemoglobin by around 10g/L. Patients given red blood cells may produce autoantibodies to donor surface antigens (of which there are many, other than ABO and RhD). Because of this, before any future transfusions, a new G&S will need to be sent (unless the last G&S was sent and processed within around 3 days of the most recent transfusion).
Platelets
- Major constituents: Platelets
- Indications – (i) Haemorrhagic shock in a trauma patient; (ii) Profound thrombocytopenia (<20 x 109/L; normal range 150 – 400); (iii) Bleeding with thrombocytopenia; (iv) Pre-operative platelet level <50 x 109/L
- Duration over which it is administered – 30 minutes
- 1 ATD (adult therapeutic dose) of platelets should increase platelet levels by around 20-40 x 109/L.
Fresh Frozen Plasma (FFP)
- Major constituents– Clotting factors
- Indications– (i) Disseminated Intravascular Coagulation (DIC); (ii) Any haemorrhage secondary to liver disease; (iii) All massive haemorrhages (commonly given after the 2ndunit of packed red cells)
- Duration over which it is administered– 30 minutes
Cryoprecipitate
- Major constituents – Fibrinogen, von Willebrands Factor (vWF), Factor VIII and fibronectin
- Indications – (i) DIC with fibrinogen <1g/L; (ii) von Willebrands Disease; or (iii) Massive haemorrhage
- Duration over which it is administered – Stat
Key Points
- Prescribing blood products should be taken seriously and with an awareness of the potential complications
- ABO and Rhesus are the two most commonly used groups for blood type classification, however other antibodies are present
- When blood is harvested from donors, it is separated into its constituent parts, which can be then given separately or concurrently, depending on the clinical situation