Introduction
Epilepsy is defined as a predisposition to seizures caused by the sudden, synchronous discharge of cerebral neurones.
It has many causes, such as primary generalised epilepsy, hippocampal sclerosis, tuberous sclerosis, cortical tumours, or infection (such as tuberculosis or cerebral abscesses).
The goal of epilepsy surgery is to lessen the frequency and/or severity of seizures or to stop seizure activity entirely.
Depending on the underlying cause, epilepsy surgery is a potential option for many patients with drug-resistant epilepsy. However, whilst techniques develop, becoming safer and less invasive, it remains an underused intervention.
Indications
Up to 30% of patients with epilepsy continue to have seizures despite optimal treatment with anti-epileptic medication. These patients with drug-resistant* (often termed refractory) epilepsy are potential surgical candidates.
When selecting appropriate patients, consideration is given not only to seizure frequency and severity but also to potential psychological and occupational improvements. For example, infrequent yet life-threatening events may be an indication for surgery, as will less-threatening seizures that have a significant psychological and occupational impact.
The possible benefits of surgery must be weighed carefully against the risk of loss of function.
*To be deemed ‘drug-resistant’ patients must have failed to achieve sustained seizure freedom despite adequate trials of two antiepileptic medications
Investigations
The success of epilepsy surgery relies on identifying patients who are likely to experience a reduction in seizure activity without suffering unacceptable postoperative neurological deficit.
Following the relevant clinical history and examination, a range of pre-surgical investigation may be warranted to further assess such cases:
- Video EEG telemetry – can be useful to identify the portion of the cortex responsible for the initiation, organisation, and propagation of seizure activity
- Deep intracranial electrodes – can be used to determine the nidus of the seizure
- MRI and Functional MRI – to identify structural lesions and determine the dominant hemisphere in certain functions respectively
- PET or SPECT – can be used to localise epileptic foci and provide information about the brain’s functional status
- Magnetoencephalography – can map brain activity by recording magnetic fields produced by electrical currents occurring in the brain
Neuropsychological & neuropsychiatric evaluation may be required also pre-operatively. This aims to assess memory, to identify any co-morbid psychiatric conditions, and to establish patient’s required level of pre- and post-operative support.
Some operations are conducted with the patient awake, particularly the removal of a space-occupying lesion (SOL) from eloquent cortex or areas adjacent to eloquent cortex. As assessment must be made as to whether the patient could tolerate such an operation without undergoing distress significant enough to render the operation non-viable.
Management
Surgical Resection
Surgical resection aims to remove the minimum amount of cortex that must be resected to achieve relative seizure freedom. This is called the epileptogenic zone.
Types of resection include:
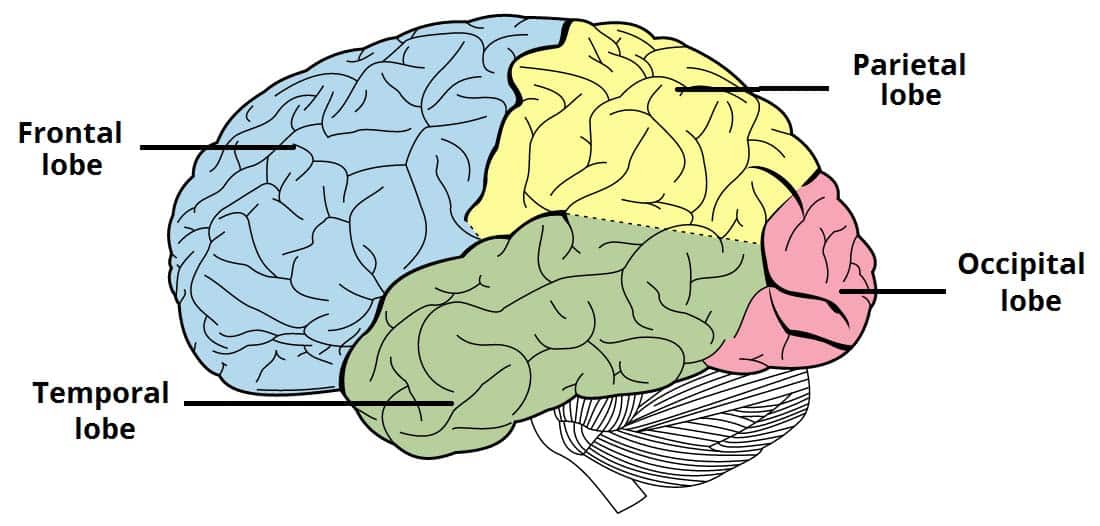
- Temporal lobectomy, whereby varying amounts of tissue become resected, ranging from the lateral temporal cortex and medial structures (e.g. hippocampal region) to only limited to the anterior temporal lobe or the medial structures (selective amygdalohippocampectomy)
- Extratemporal resection, whereby dysfunctional tissue is removed from areas outside the temporal lobe
- Lesionectomy, involving removal of a discrete lesion, such as an abscess or tuberculoma
- Corpus callosotomy, where the corpus callosum is cut to prevent the spread of seizure activity from one hemisphere to the other
- Multiple subpial transection, required if the epileptogenic zone is located in an inoperable part of the brain, then the connections to the epileptic focus are cut without resecting tissue
Resective surgery (and deep brain stimulation) are associated with specific complications that may develop, including infection, bleeding (including subgaleal haematoma), visual field defects or dysphasias, hemiparesis, and memory disturbances.
Less Invasive Surgical Techniques
Vagal Nerve Stimulation and Deep Brain Stimulation are two potential additional surgical options for epilepsy which do not involve resection or transection. They are often used in cases where resective surgery is not appropriate or has not been successful (or also as an adjunct to anticonvulsant therapy).
In vagal nerve stimulation, a battery generator (similar to a pacemaker) is implanted in the left upper chest and connected to the left cervical vagus nerve, which then delivers regular impulses to the vagus nerve. These impulses modulate neurotransmitter release in afferent vagal synapses, helping (in theory) to desynchronise cerebral cortical activity and thus reduce seizure activity.
In deep brain stimulation, a battery-operated neurostimulator sends impulses to electrodes that have been implanted directly in the brain. The electrodes are often placed in the anterior nucleus of the thalamus or in the hippocampus, areas which are frequently epileptogenic and aids to dampen the spread of seizure activity.
Key Points
- Epilepsy surgery has potential in refractory epilepsy, however is often underused
- Several investigations are used concurrently to identify the area responsible for generating seizures prior to any intervention
- The goal of surgery is resection or electrical stimulation of the epileptic focus without causing unacceptable neurological deficit