Introduction
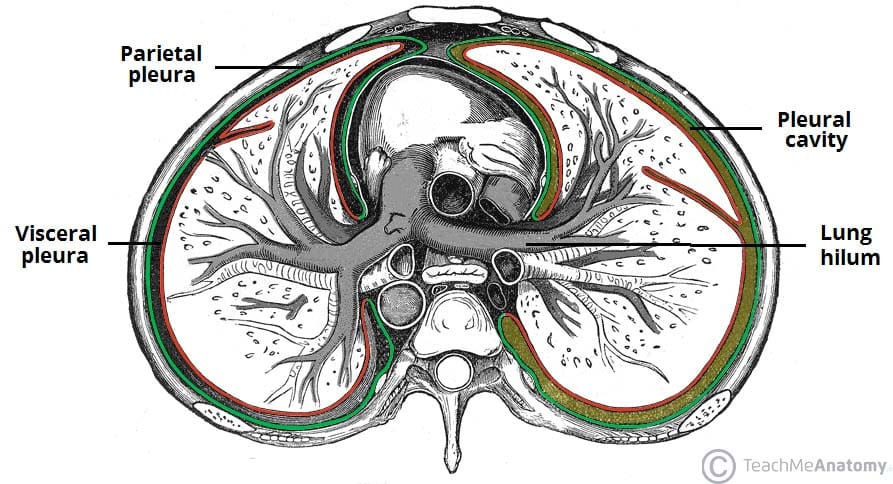
A pneumothorax is the presence of air within the pleural cavity. This is usually from a defect on the lung surface (e.g. rupture bullae) or through damage to the chest wall (e.g. following trauma).
Air within the pleural cavity causes the physiological pleural seal to be lost, meaning the normal negative pressure in this space, that aids the lung expanding with chest wall movement, is lost. This impedes lung expansion and lead to partial or total lung collapse (Fig. 1).
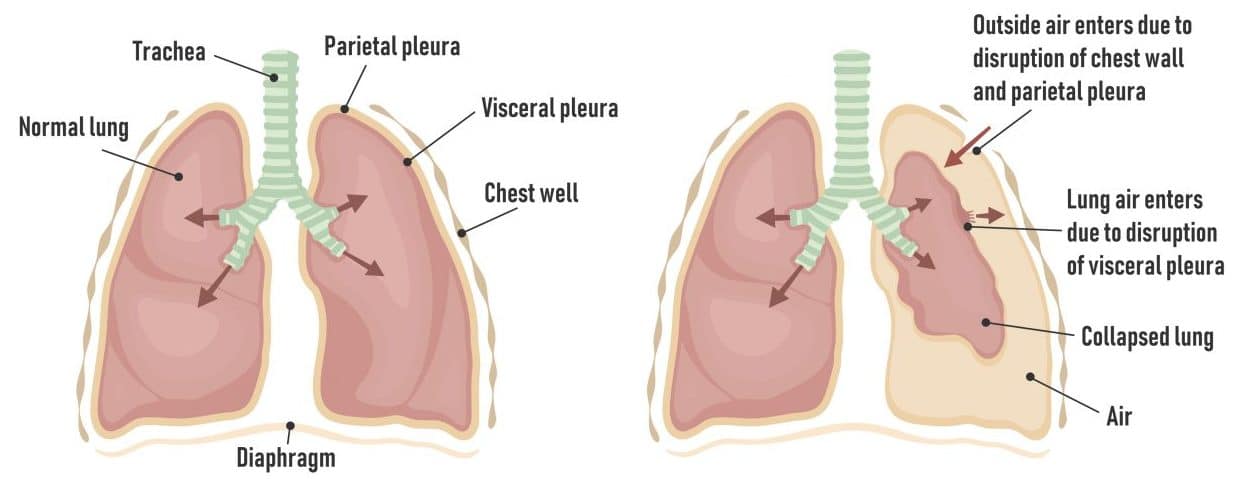
Figure 1 – Schematic showing normal thorax anatomy (left) and pathology occurring in a pneumothorax (right)
Tension Pneumothorax
A tension pneumothorax is a pneumothorax with a progressive accumulation of air within the pleural space, leading to cardiorespiratory compromise. Air becomes becomes trapped in the pleural space, leading to a positive pressure, often described due to a one-way valve developing.
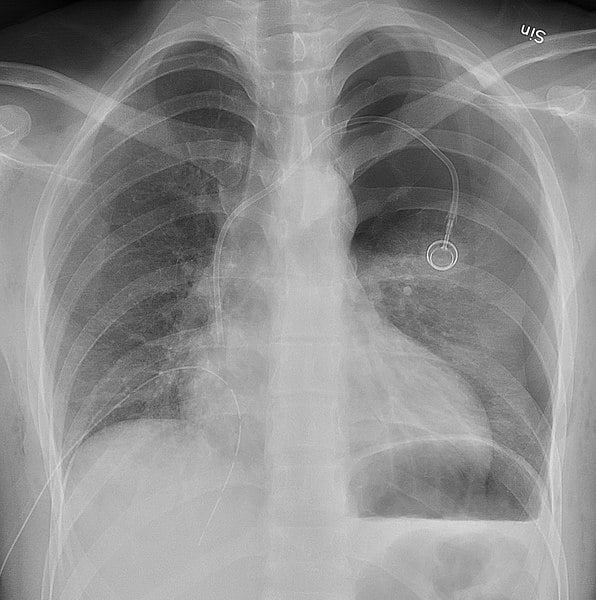
If left untreated, this positive pressure causes mediastinal shift (Fig. 2), pressure on venous return to the heart, and can result in eventual cardiac arrest. Patients with a tension pneumothorax will often present in extremis and require urgent decompression.

Figure 2 – Plain film chest radiograph showing a left-sided tension pneumothorax with mediastinal shift
Classification
The two main types of pneumothorax are:
- A spontaneous pneumothorax, which can be either:
- Primary, whereby no underlying cause is identified; commonly seen in young, tall, and thin males (especially if a smoker)
- Secondary, where there is underlying lung disease; most commonly in COPD patients from a ruptured bullae
- A traumatic pneumothorax occurs in the context of a traumatic chest injury, such as a stab injury or a fractured rib
- Includes iatrogenic causes, such as central line insertion or mechanical ventilation
Clinical Features
The majority of pneumothorax will present with shortness of breath, of varying degree depending on size of the pneumothorax and patient factors (such as known lung disease or physiological reserve).
This can be accompanied by sudden onset chest pain, often pleuritic in nature. Small spontaneous pneumothorax can be asymptomatic, particularly in younger patients.
On examination, there will be hyperresonance on percussion, reduced / absent breath sounds on auscultation, and reduced chest expansion. In cases of tension pneumothorax, patients will be hypoxic, tachycardic, and hypotensive, with potential distended neck veins and tracheal deviation away from the affected side.
Investigations
All patients with suspected pneumothorax should be approached in an A to E manner. Initial investigations should run alongside this (except for cases of tension pneumothorax, when urgent needle decompression is required).
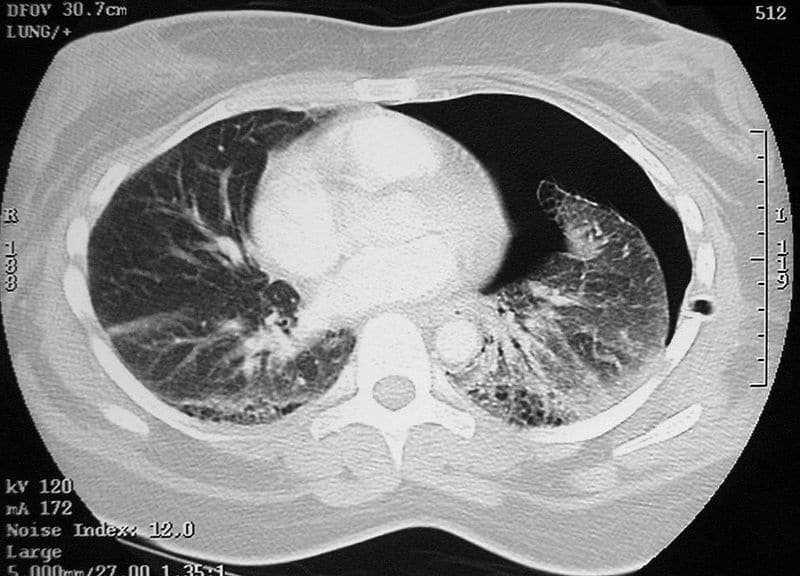
The mainstay of initial investigation is via plain film chest radiograph (CXR, Fig. 4), performed in an expiratory phase +/- lateral view. The size of a pneumothorax is determined by measuring the interpleural distance at the level of the hilum.
Other investigations required includes routine bloods (FBC, CRP, U&Es, and clotting), an arterial blood gas (ABG), and an ECG. CT imaging (Fig. 5) is not always required, however can help determine an underlying cause and, in the context of trauma, any concurrent injuries.
Management
Management will be influenced by both size and type of the pneumothorax and patient factors. As a minimal, ensure all patients have sufficient analgesia and started on oxygen if required.
For any patient with a chest drain inserted, ensure it is attached to an underwater seal. All such patients should be seen by the respiratory team ideally within 24hrs of admission.
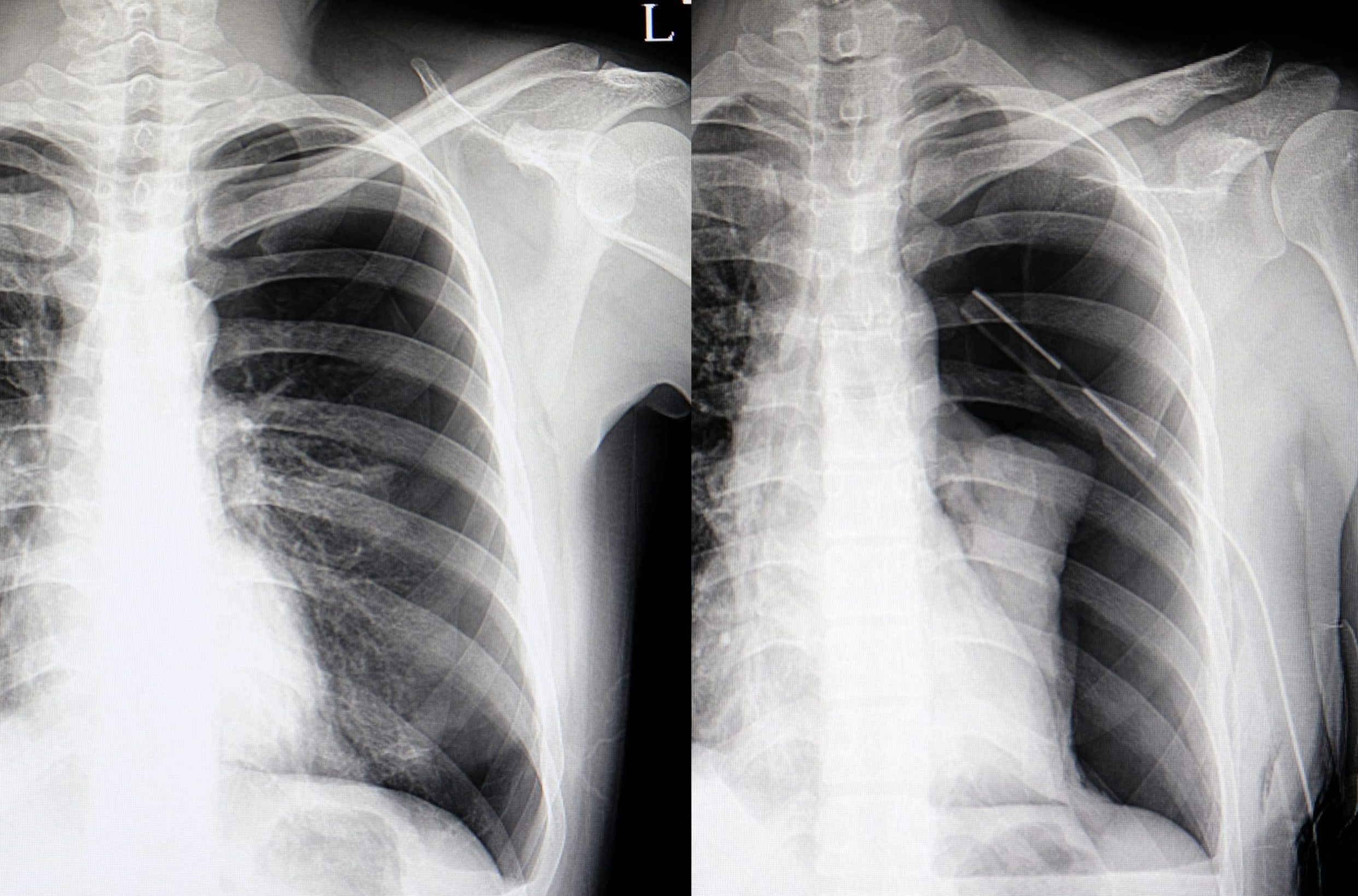
Figure 6 – Plain film chest radiograph showing a spontaneous pneumothorax (left) and then following chest drain insertion (right)
Initial Management
For primary spontaneous pneumothorax, those that are small (<2cm) and in asymptomatic patients can often be admitted for observation alone and discharged after 24hrs if remaining stable.
For symptomatic or large primary pneumothoraces, needle decompression should be attempted, placed in 2nd or 3rd intercostal space at the mid-clavicular line. If no improvement, a chest drain, via Seldinger technique, should be placed.
Small secondary spontaneous pneumothorax will require admission for observation, with a low threshold for attempting needle decompression. Those that are large and symptomatic require a chest drain, via Seldinger technique, to be placed.
Traumatic pneumothoraces will normally require a surgical chest drain insertion (Fig. 6), placed in the Triangle of Safety (Fig. 7), or otherwise admitting for observation if small and asymptomatic; importantly, there is no role in needle decompression in traumatic non-tensioning pneumothoraces*.
*For traumatic tension pneumothoraces, either needle decompression (in 5th intercoastal space mix-axillary line) or finger thoracostomy is required, prior to chest drain insertion
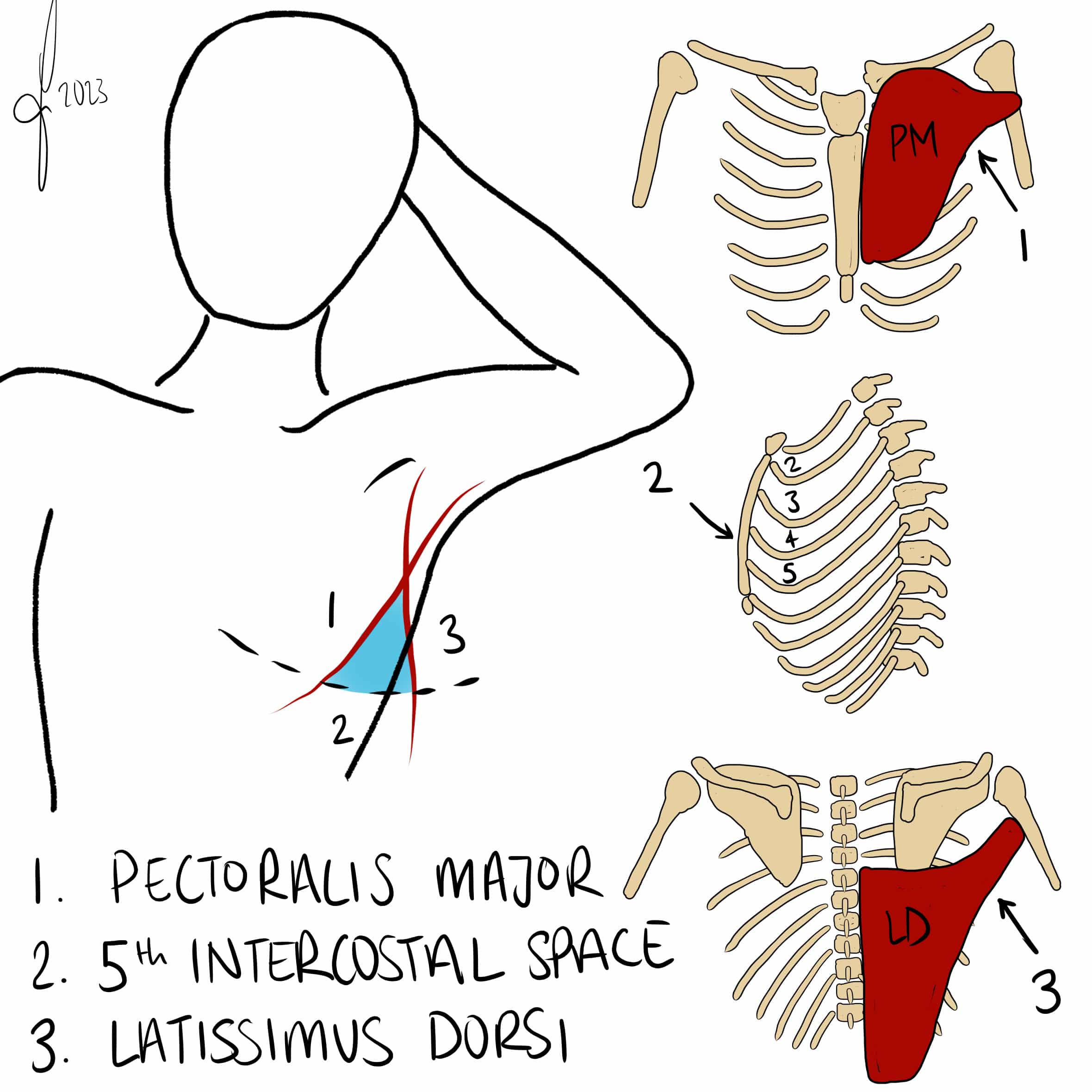
Figure 7 – The “Triangle of Safety” for insertion of a chest drain
Tension Pneumothorax
Initial management of suspected tension pneumothorax should be needle decompression with high-flow oxygen, then subsequent chest drain insertion.
Needle decompression involves inserting a large-bore cannula into the pleural cavity through the 2nd intercostal space mid-clavicular line or 5th intercostal space mid-axillary line. A subsequent hiss of air confirms the diagnosis.
Following chest drain insertion, a CXR must be performed; any persisting pneumothorax or clinical instability warrants discussion with a thoracic surgeon
Further Management
Further intervention is considered in those with a persistent air leak or failure of lung re-expansion.
In spontaneous cases, medical pleurodesis is often trialled, which results in the partial obliteration of the pleural space through the introduction of an irritant agent, aiming to prevent recurrences. Alternatively, a Heimlich valve can be trialled, a one-way valve that is attached to a chest tube and enables complete evacuation of air that is not under tension.
Those failing these interventions, or in traumatic cases, should be considered for surgical intervention. This includes either video-assisted thoracoscopic surgery (VATS) for pleurectomy +/- pleural abrasion, or open thoracotomy and pleurectomy
Key Points
- A pneumothorax occurs when air entering into the pleural space
- They can be either spontaneous, divided into primary or secondary, or traumatic
- Patients present with dyspnoea +/- pleuritic chest pain
- Diagnosis is made mainly via a plain film chest radiograph
- Cases will either require observation, or needle decompression or chest drain insertion