This article is for educational purposes only. It should not be used as a template for consenting patients. The person obtaining consent should have clear knowledge of the procedure and the potential risks and complications. Always refer to your local or national guidelines, and the applicable and appropriate law in your jurisdiction governing patient consent.
Overview of Procedure
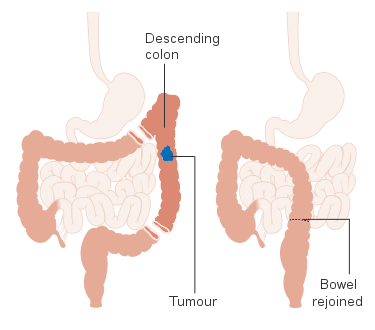
A left hemicolectomy involves the removal of the splenic flexure, descending colon, and a portion of the sigmoid colon.
Left hemicolectomies can be done either open or laparoscopically, and either electively or in an emergency. In the majority of cases, an anastomosis from the transverse colon to the sigmoid colon is formed during the indexed procedure; in uncommon circumstances, a defunctioning ileostomy may be formed, especially if there are concerns regarding the anastomosis
Left hemicolectomies are most commonly performed for bowel malignancy, but can also be performed for diverticular disease, bowel ischaemia, or bowel perforation. Left hemicolectomies are slightly less common then right hemicolectomies, as fewer bowel cancers occur in the descending colon compared to the ascending colon
Complications
Intra-Operative
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Bleeding | Ensure meticulous haemostasis during the procedure; careful dissection at the splenic flexure off the spleen | |
| Damage to local structures | Structures at risk include small bowel, kidney + bladder + ureter, and spleen; if the splenic flexure is densely adherent to the spleen, splenectomy may be required | |
| Anaesthetic risks | Includes damage to the teeth, throat and larynx, reaction to medications, nausea and vomiting, cardiovascular and respiratory complications. | Forms part of anaesthetic pre-assessment |
Early
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Pain | Pain is often worse in open procedures, compared to laparoscopic | Optimal post-operative analgesia, including epidurals or rectus sheath catheters |
| Infection | Includes both wound infections and intra-abdominal collections, as well as respiratory or urinary tract infections post-operatively | Intravenous antibiotics at induction, minimisation of faecal contamination during procedure, wound irrigation at closure |
| Anastomotic leak | Good blood supply at the anastomosis, bowel not under tension | |
| Ileus | Minimise contamination and bowel handling, correct any electrolyte abnormalities post-operatively | |
| Scarring | Use of laparoscopic surgery if possible to result in a smaller scar | |
| Re-Operation | Any complication may result in the return to theatre in the immediate post-operative period | |
| DVT or PE, Myocardial Infarction, Stroke, or Mortality | As with any major surgery, whilst these events are uncommon, important to be aware of | Adequate pre-optimisation and anaesthetic assessment, peri-operative prophylactic LMWH, high-dependency level care post-operatively |
Late
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Adhesions | Attempt laparoscopic approach if possible, avoid excess tissue disruption | |
| Stoma complications | Includes stoma retraction, prolapse, or high stoma output, if a stoma is formed | |
| Incisional hernia | Ensure fascia is closed tightly, using a small bites technique |