Introduction
Lung transplantation is the benchmark therapy for end-stage pulmonary failure, where all other treatment modalities have been exhausted or are not deemed suitable.
The demand for donor lungs from deceased donors still outweighs the supply, however the number of lung transplants performed has slowly increased in a few high-income countries in recent years. In the UK, there are approximately 200 heart or heart and lung transplants a year.
Patients awaiting their transplants are managed using bridges to transplantation devices, such as ventricular assist devices (VAD) and extracorporeal membrane oxygenation (ECMO).
Indications
The most common conditions that may be indications for lung transplantation are end-stage chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, cystic fibrosis, and bronchiectasis.
Whilst this can vary from centre to centre, lung transplantation is considered when the patient has a high risk of death (>50%) from lung disease within 2 years if lung transplantation is not performed. The patient must also have a high likelihood of surviving (>80%) at least 90 days after lung transplantation.
The main contraindications for lung transplantation include active malignancy, significant dysfunction of another major organ system (unless a combined transplantation is being considered), chronic infection (including active TB), or a significant chest wall or spinal deformity.
Surgical Techniques
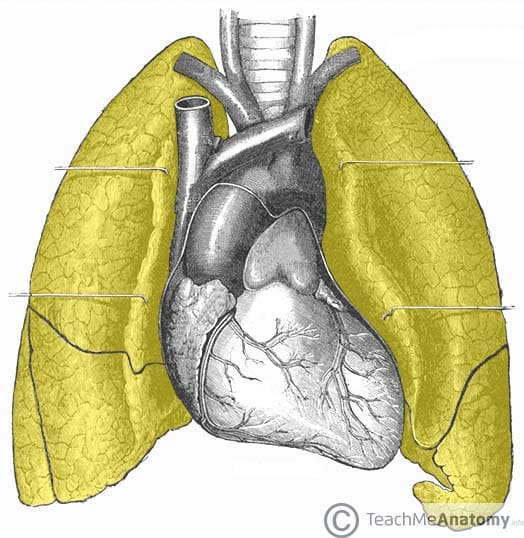
Donor lungs come exclusively from deceased donors, with the prospective donors matched using blood group, HLA status, and expected lung capacity. Lung transplantation can be either single or double lung* transplantation, and can also occur (rarely) as a combined procedure via a heart and lung transplantation
*Double lung transplantation can either be performed as single lung transplantation bilaterally (preferred) or can be performed where both lungs are transplanted simultaneously (i.e. an en-bloc procedure).
Donor Procedure
The lungs are retrieved* following heart retrieval and are gentle ventilated to reduce atelectasis. The lungs are dissected from the pulmonary ligaments and the pulmonary vessels are flushed with heparinised solution. Typically the right lung is freed first, before the left lung is subsequently freed.
The remaining pericardium is then left intact with the left atrium and the pulmonary veins, as well as the pulmonary artery above its bifurcation. The lungs are inflated prior to stapling across the divided trachea and then removed in their anatomical position. They are placed onto ice-cold storage or attached to an ex-vivo lung perfusion system.
*The process is the same in DCD but the airway must be protected as a first priority, and assessment of the lungs must be done promptly after sternotomy the minimise warm ischaemic time
Recipient Procedure
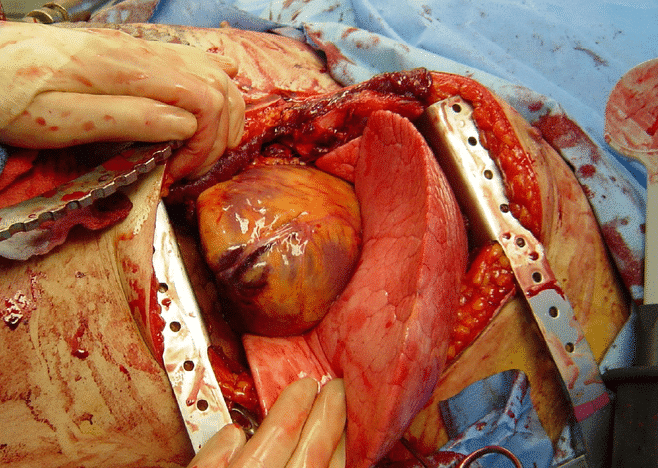
Lung implantation can occur by a variety of incisions; typically anterior thoracotomies are used (Fig. 2), however a lateral thoracotomy incision may be used for single lung transplants. Cardiopulmonary bypass will be used.
Once the diseased lungs are removed, the donor lung(s) are placed into the chest and the anastomoses is performed in the sequence of bronchus, left atrium (with the pulmonary veins still preserved), and pulmonary artery.
Complications
Early
In the initial days following the procedure, patients are at risk of both reperfusion injury and primary graft dysfunction, often requiring ECMO during this period.
Due to immunosuppressed status, post-operative infections are common. Dehiscence of the bronchial anastomoses can occur, causing an air leak into the mediastinum
Late
Due to the immunosuppression and disrupted muco-ciliary clearance mechanisms, patients remain at lifelong risk for infections of recurrent or atypical infections, as well as nephrotoxicity and malignancies (including post-transplant lymphoproliferative disorder)
Lung transplant patients are at risk of developing bronchiolitis obliterans syndrome, where there is severe damage to the bronchioles and typically occurs within the first year following transplantation.
Key Points
- Lung transplantation is the benchmark therapy for end-stage pulmonary failure
- Indications for lung transplantation include end-stage COPD, pulmonary fibrosis, cystic fibrosis, and bronchiectasis
- Lung transplantation can be either single or double lung transplantation, and can also occur as a combined procedure via a heart and lung transplantation
- Due to immunosuppressed status, post-operative infections are common