Introduction
Liver transplantation (LT) is indicated for the treatment of acute liver failure (ALF) and end-stage liver disease (ESLD). Currently, the overall 1-year and 5-year post-LT patient survival rates are 80-90% and 60-75%, respectively.
Liver transplantation can be classified according to the type of donor, into deceased and live donor liver transplants.
Liver grafts in the Western countries come predominantly from deceased donors in around 95% of the cases*. Orthotopic liver transplantation (OLT) is by far the most common procedure, where the native liver is removed then replaced by the donor liver in the same anatomic position.
Whilst most liver transplants are of the whole organ, segmental liver transplantation or reduced graft can also be performed.
- Segmental (or split) liver transplantation allows transplanting two recipients (commonly an adult and a child) with a single cadaveric organ
- Reduced grafts accommodates for cases with a mismatch between the size of the donor and the recipient
*Live liver donation, whereby only part of the liver is transplanted from a living donor, constitutes the major source for organ donation in the Far East (e.g. Japan and Korea) and in some other countries where cultural beliefs and customs regarding burial after death limit transplantation from deceased donors of whole organs
Indications
The most common indications for liver transplantation in Western countries are end-stage liver disease (ESLD) due to chronic HCV infection, alcoholic liver disease (ALD), or non-alcoholic fatty liver disease (NAFLD).
Other conditions include:
- Non-cholestatic liver disorders
- Chronic HBV infection, autoimmune hepatitis, or cryptogenic
- Cholestatic liver disorders
- Primary biliary cirrhosis (PBC) or Primary sclerosing cholangitis (PSC)
- Metabolic liver disorders
- Alpha-1-antitrypsin deficiency, Wilson’s disease, hereditary hemochromatosis, or Crigler–Najjar syndrome
- Primary malignancies of the liver
- Hepatocellular carcinoma, hepatoblastoma, or hilar cholangiocarcinoma
- Budd-Chiari syndrome
- Drug-induced acute liver failure
The severity of the end-stage liver disease can be evaluated with the Model for End-Stage Liver Disease (MELD) scoring system, calculated from the patient’s INR, bilirubin, creatinine, and sodium, estimating patient survival and is used to prioritise patients on the transplant waiting list.
Acute liver failure, defined as severe encephalopathy and coagulopathy in the absence of pre-existing liver disease, can be classified by the King’s College Criteria, also helping to identify the patients that will most benefit from LT.
Contraindications
Contraindications to liver transplantation can be divided into absolute and relative.
|
Absolute |
Relative |
| Uncontrolled sepsis
Active alcohol or substance abuse, or persistent non-adherence to medical therapy Advanced cardiac or pulmonary disease Extra-hepatic malignancy |
Multi-system organ failure with fulminant liver failure
Active infection Advanced age, frailty, or extensive co-morbidities Medication-resistant HBV cirrhosis |
Table 1 – Contraindications to liver transplantation
Surgical Techniques
The two key steps of LT are organ retrieval and recipient implantation. Donor-recipient matching is mainly based on ABO compatibility and graft to recipient weight ratio (GRWR). HLA-based compatibility is not essential for LT.
Donor Procedure
The organ retrieval pathway differs according to the type of deceased donation. This can be classified into donation after Donation after Brainstem Death (DBD) or Donation after Circulatory Death (DCD).
DBD Retrieval
For a liver retrieval from a DBD donor, full exposure of the abdomen and the chest is obtained with a midline laparotomy and thoracotomy. The liver is mobilised and the common bile duct is dissected, with the gallbladder emptied and flushed. The donor is heparinised and cold preservation fluid instilled systemically, before the descending thoracic aorta is cross-clamped.
The liver is rapidly removed from the body with the common hepatic artery left in continuity with the celiac axis on an aortic patch. The infra-hepatic and supra-hepatic IVC are cut to allow the liver to be retrieved with the whole IVC beneath it. The organ is taken out of the body, placed on ice on a back table for further portal perfusion, before transportation.
DCD Retrieval
For a liver retrieval from a DCD donor, once asystole is confirmed, a rapid laparotomy and thoracotomy are performed. The aorta is cross-clamped and cold perfusion fluid is instilled via the cannulated aorta, to minimise warm ischaemia time. Portal perfusion is established through a portal vein cannula. The remainder of the procedure is then equivocal to the cold phase dissection in the DBD donor.
Recipient Procedure
The recipient procedure is composed of two steps; the hepatectomy and the liver graft implantation.
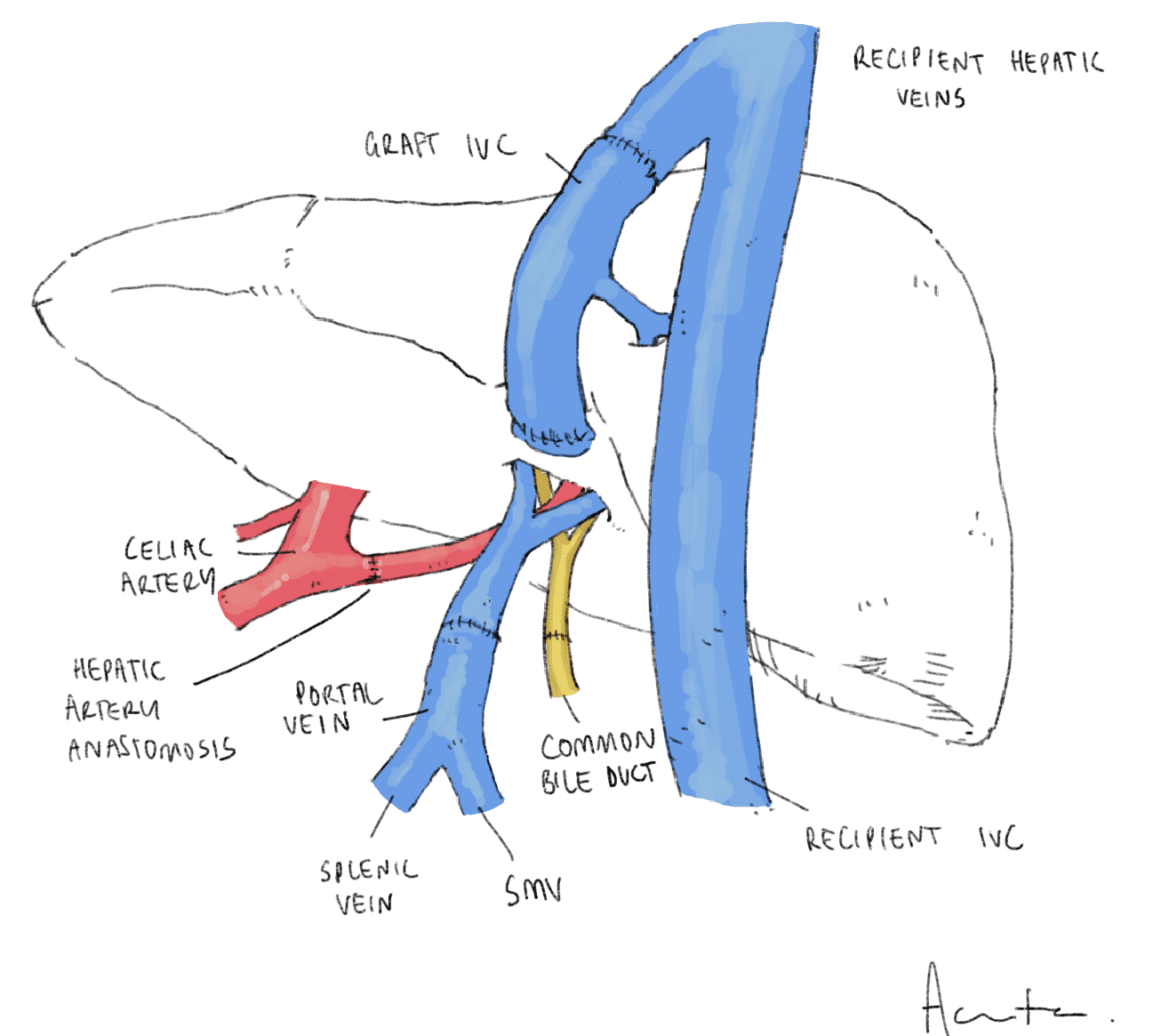
Two types of hepatectomy exist, the classic approach (Fig. 3) with the excision of the recipient IVC or the piggyback technique (Fig. 4) with IVC preservation. The classic approach is characterised by an interruption of the venous return with significant haemodynamic changes, therefore piggyback technique is often opted for where feasible.
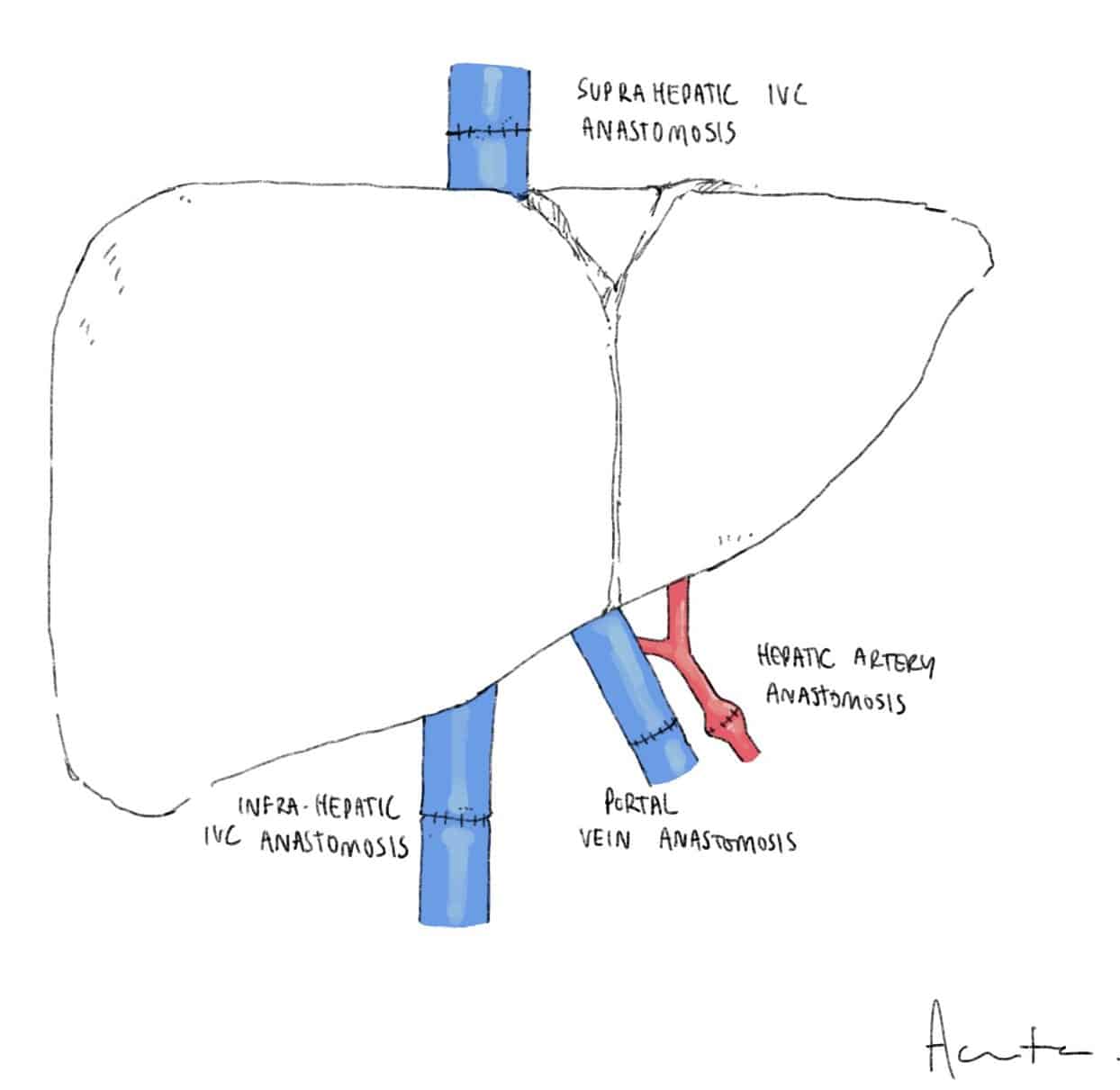
Figure 3 – Illustration demonstrating the classical recipient liver transplant technique
According to the type of hepatectomy chosen, the implantation will then be either a cava replacement transplant or piggyback implantation. In case of the piggyback implantation, the donor IVC can be attached to the recipient IVC side-to-side or the suprahepatic end anastomosed to the recipient hepatic veins.
In both cases, the portal veins and hepatic arteries of the donor and recipient are anastomosed end-to-end. The preferred type of biliary anastomosis is duct-to-duct or a Roux-en-Y hepaticojejunostomy (such as in PSC patients as the recipient bile duct is diseased).
Complications of Liver Transplant
Complications following LT are common and the mortality rate within the first year is 5-10%. Postoperative haemorrhage is the most common surgical complication (15%).
Graft Primary Non-Function
The most severe form of graft dysfunction is primary non-function, an extreme form of preservation injury that prevents the recovery of the graft after revascularisation. Its incidence varies between 1-3%.
It clinically manifests as an acute liver failure with jaundice, coagulopathy, encephalopathy, and raised serum aminotransferase levels, in the absence of vascular complications.
Prolonged cold ischaemia time, prolonged warm ischaemia time in DCD grafts, and fatty liver grafts are the major risk factors. Re-transplantation is the only current therapeutic option.
Vascular Complications
The most common vascular complications following LT are hepatic artery thrombosis (HAT), portal vein thrombosis (PVT), and venous outflow obstruction:
- HAT is the most common vascular complication post-LT, typically occurring at the anastomotic site between donor and recipient hepatic artery, presenting with graft failure
- Doppler ultrasound can detect HAT and the diagnosis can be confirmed with CT arteriography; therapeutic options range from interventional endovascular techniques to surgical revision or re-transplantation
- PVT presents either with graft failure (if early PVT) or with signs of portal hypertension (if late PVT)
- Diagnosis is also made using Doppler ultrasound and CT portography (Fig. 5); surgical revision and re-transplantation will be required in early cases, but late cases can often be managed conservatively
- Obstruction of the IVC outflow is rare, with trans-jugular cavogram and pressure gradient measurements to help establish the diagnosis; endovascular intervention with stenting or balloon angioplasty is often the treatment of choice
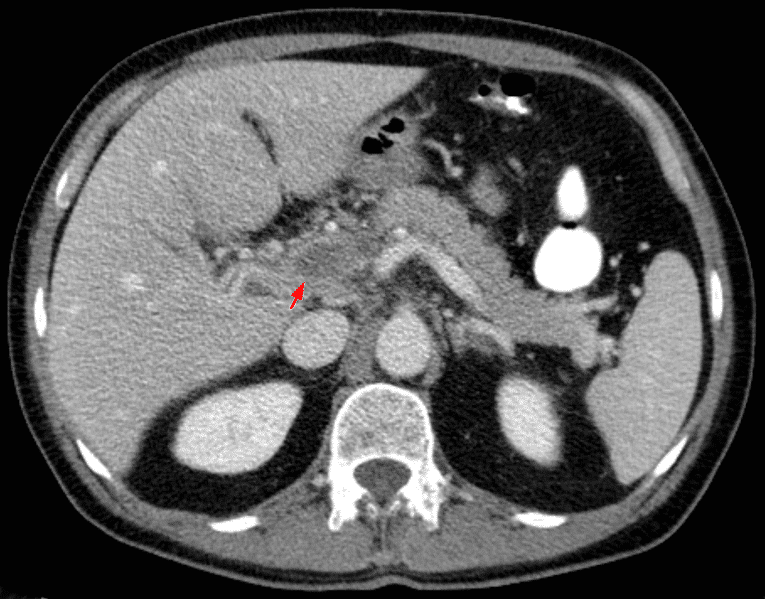
Figure 5 – A portal vein thrombus (arrow), as seen on CT imaging
Biliary Complications
Biliary complications include leaks or strictures and occur in 10-20% of LTs, the majority occurring within the first three months of transplantation.
Bile leak is almost always seen in the early postoperative period and the patients may develop signs of localised peritonitis or sepsis.
Biliary strictures can be categorised as anastomotic or non-anastomotic (ischaemic cholangiopathy):
- Anastomotic biliary strictures present late in the post-operative period, with progressive cholestasis; MRCP can confirm the diagnosis and ERCP plus stenting or dilatation is often the treatment of choice
- Ischaemic cholangiopathy involves segmental stenosis of the biliary tree, with the main risk factor being long cold ischaemia time; treatment can be difficult and re-transplantation may be required indicated if widespread
Rejection
Acute rejection episodes occur in about 25-50% of liver transplant recipients in the first year after transplant. They are usually diagnosed with deranged liver function tests in the follow-up period, which needs to be confirmed with a liver biopsy.
Treatment depends on the severity of acute rejection and ranges from immunosuppression dose modifications up to high dose intravenous corticosteroids or polyclonal antibodies.
Long-term Complications
Other complications of LT include systemic hypertension (as well as ischaemic heart disease), de novo diabetes mellitus (often secondary to glucocorticoid or long-term calcineurin inhibitor use), renal impairment (also due to calcineurin inhibitor use poor glycaemic control), dissemination of undetected donor diseases (infection or malignancy), recurrence of the primary liver disease, and chronic rejection.
Key Points
- Liver transplantation is indicated for the treatment of acute liver failure and end-stage liver disease
- The majority of liver transplants are via orthotopic liver transplantation (OLT), whereby the native liver is removed then replaced by the donor liver in the same anatomic position
- Rejection, biliary complications, and vascular complications (including bleeding) form the mainstay of post-operative complications
- Five year survival rates post-liver transplantation are 60-75%