Introduction
Lung cancer is the third most common cancer in Western countries and is the most common cause of cancer-related death. 5-year survival rates are low, at approximately 16%, with survival rates higher in females. Worldwide, lung cancer causes around 2 million deaths each year.
Classification
Lung cancers are classified into two main categories: small cell (15-20% of total) or non-small cell (80-85%) carcinoma (Fig 2).
Small cell carcinomas originate from neuroendocrine cells. Small cell carcinomas generally develop centrally near a main bronchus and have a strong association with smoking. They grow quickly and metastasise rapidly in comparison to non-small cell lung cancers.
Non-small cell carcinomas are further subdivided into (1) squamous cell (square shaped cells that produce keratin), (2) adenocarcinoma (form glandular structures that produce mucin), (3) carcinoid tumours (from mature neuroendocrine cells) or (4) large cell (lack glandular and squamous differentiation).
Squamous cell carcinomas also develop centrally and have a strong association with smoking. Adenocarcinomas develop peripherally in a bronchial or alveolar wall, also associated with smoking and more common in women. Large cell carcinomas are found throughout the lung, centrally or peripherally.
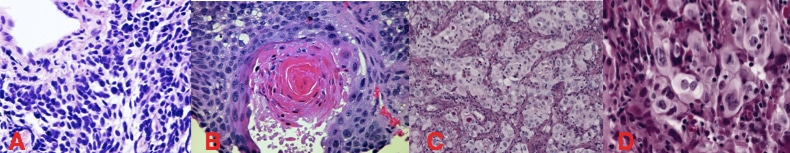
Figure 2 – Histological appearances of lung cancer subtypes (A) small cell carcinoma (B) squamous cell carcinoma (C) adenocarcinoma (D) large cell carcinoma
Risk Factors
Smoking is the biggest risk factor, with 90% of lung cancers diagnosed in smokers; the risk is dose dependent and increases with increasing amount of cigarettes smoked and time.
Other risk factors include asbestos exposure, air pollution, exposure to Radon gas, and exposure to ionising radiation (such as repeated CT imaging).
Clinical Features
Symptoms depend on type of lung cancer, location of primary tumour, and extent of any metastatic spread.
Local symptoms will include cough, haemoptysis, and shortness of breath. Constitutional symptoms can become present in more advanced disease, which include unintentional weight loss, malaise, and fatigue.
Distant metastases commonly occur to the brain (symptoms vary depending on location such as personality changes in frontal mets), liver (abdominal pain from stretch to the liver capsule), bone (bone pain or pathological fractures), or adrenal glands.
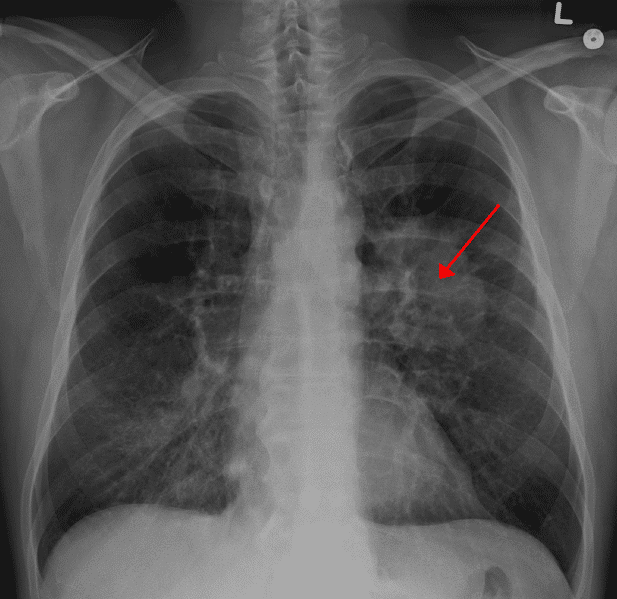
Figure 4 – Plain film radiograph showing a lung cancer (arrow)
Local Invasion
Invasion of the tumour into surrounding mediastinal structures can also result in clinical features.
Apical tumours, often termed Pancoast tumours (typically non-small cell lung cancer) can compress on the brachial plexus, producing upper limb paraesthesia or weakness, on the (stellate ganglion of the) cervical sympathetic chain, resulting in a Horner’s syndrome, which can present with ptosis, meiosis, and / or facial anhidrosis (Fig. 5).
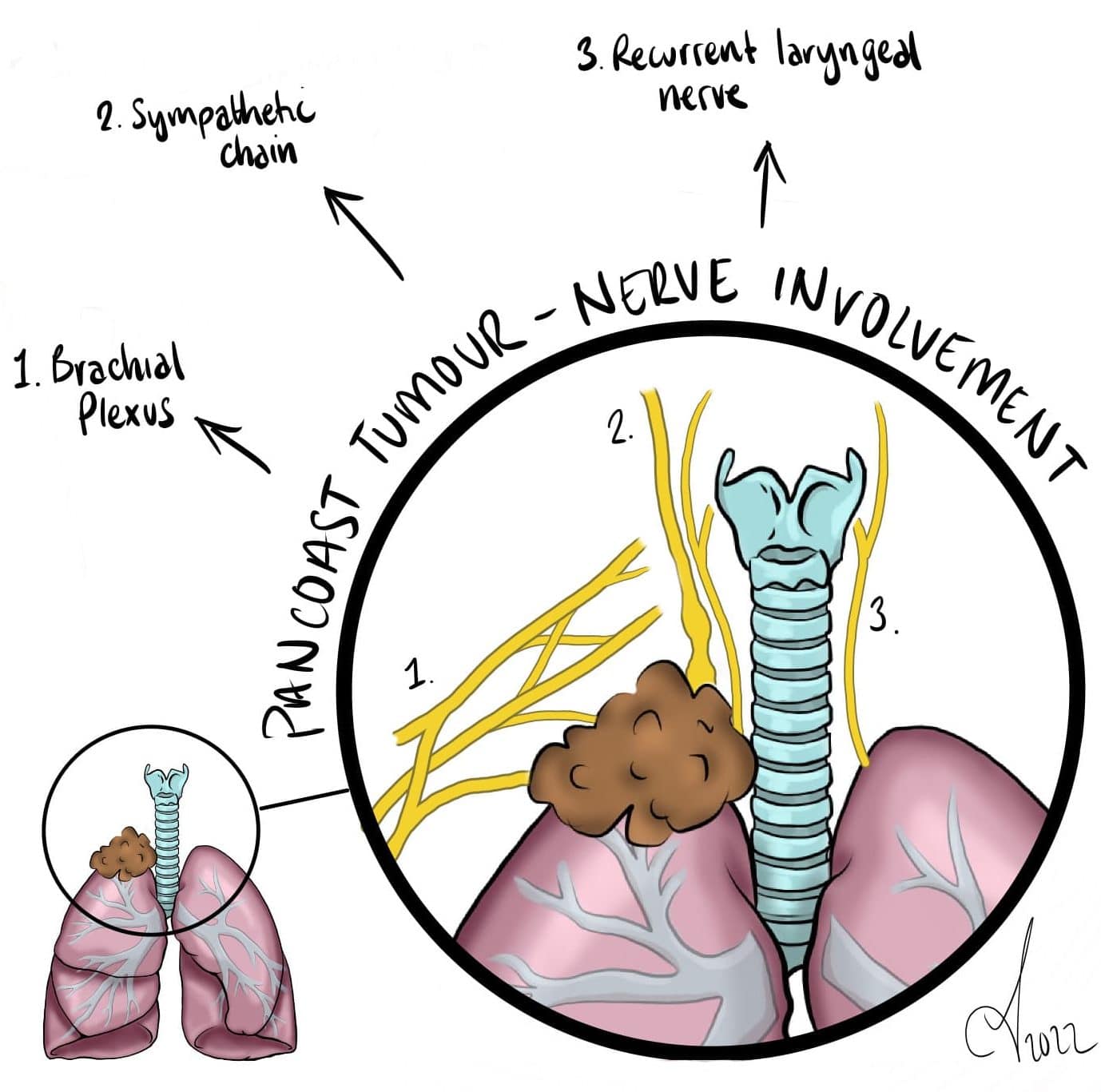
Figure 5 – Illustration demonstrating a Pancoast Tumour resulting in nerve involvement
Compression on the phrenic nerve, leading to paralysis of the ipsilateral hemidiaphragm, can cause further respiratory compromise. Compression of recurrent laryngeal nerve can present with hoarse voice. Compression of the superior vena cava (SVC obstruction) can cause facial plethora (Fig. 6), prominence of facial and/or upper limbs veins, and respiratory compromise (Pemberton’s sign).
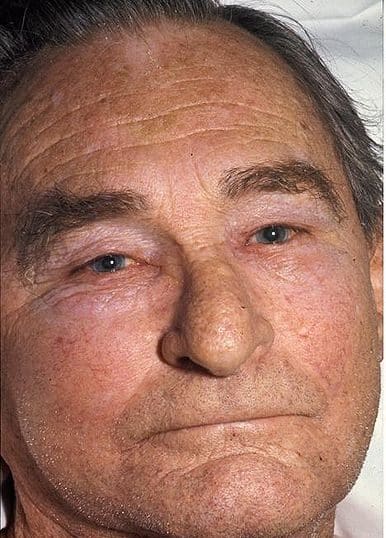
Figure 6 – Facial swelling, as seen in SVC syndrome
Paraneoplastic Syndromes
Squamous cell lung cancers can produce parathyroid hormone-related peptide (PTHrP), which can mimic the function of parathyroid hormone (PTH), leading to clinical features of hypercalcaemia.
Adenocarcinoma can cause hypertrophic osteoarthropathy that can present with clubbing, joint pain, and bone pain.
Small cell lung cancers can produce anti-diuretic hormone (ADH) that can lead to syndrome of inappropriate antidiuretic syndrome secretion (SIADH), resulting in hyponatraemia. They can also produce adrenocorticotropic hormone (ACTH) that can results in Cushing’s syndrome.
Antibodies against the presynaptic calcium channel of the neuromuscular junction can also be produced by small cell lung cancers, resulting in a Lambert-Eaton syndrome, which can present with proximal muscle weakness.
Differential Diagnosis
Differential diagnoses for patients with local symptoms of lung cancer include pneumonia, pulmonary tuberculosis, pulmonary embolism, or cardiac failure
Investigations
Any patient presenting with suspected lung cancer should have blood tests, specifically inflammatory markers (FBC and CRP, to exclude infectious causes), urea & electrolytes (U&Es), and bone profile.
The majority of patients will initially have a plain film chest radiograph (Fig. 4), which may show a nodule or mass (or any sequelae of metastatic spread). However, a contrast CT chest scan should be performed (Fig. 7), to better characterise a lesion and to check for the presence lymph node involvement or local invasion.
For confirmed cases, subsequent staging imaging is required, with staging PET-CT (for NSCLC) or CT abdomen-pelvis (for SCLC) +/- CT head (if considered for curative intent)

Figure 7 – CT scan showing a lung cancer in the left upper lobe
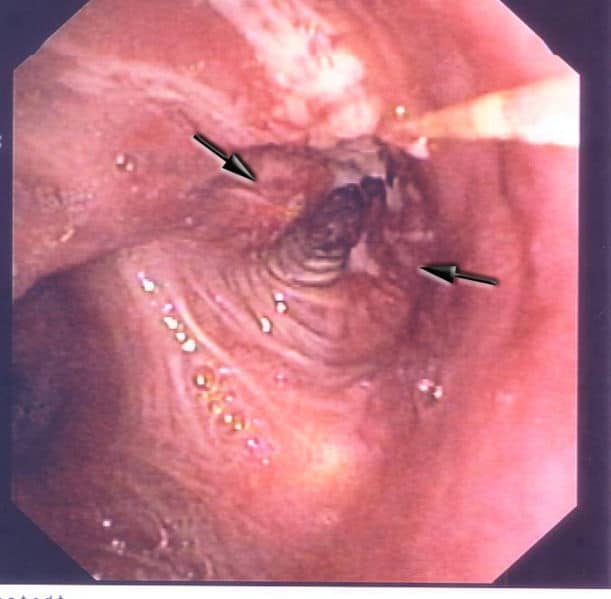
Biopsy Options
A centrally-located tumour can then be biopsied either with a transbronchial biopsy (if the tumour is within the lumen) or ultrasound-guided endoscopic biopsy (if the tumour is outside of the lumen). If the tumour is located peripherally, a transthoracic approach may be required (either via CT-guided biopsy or a video-assisted thoracoscopic surgical approach).
Patients presenting with a pleural effusion will often undergo a diagnostic thoracocentesis; the pleural fluid should be sent for cytology (to check for malignant cells), alongside cell count, microscopy, culture, glucose, LDH, and protein. This can help differentiate between a transudate and exudate; if inconclusive, then Light’s criteria can be used to confirm
Management
All patients with lung cancer should be discussed at the appropriate multidisciplinary team meeting (MDT). Management will be determined by both disease factors and patient factors.
Chemotherapy +/- radiotherapy will form the mainstay of management for metastatic lung cancer. Prophylactic radiotherapy to the brain can be performed, especially for small-cell lung cancer, as they have often metastasised at time of presentation. Newer immunotherapy agents can also be of benefit, especially in non-small cell lung cancer.
Surgical Management
Surgical resection is the only definitive curative treatment options. A lobectomy is the standard approach* for most non-small cell lung cancers, however this will differ depending on the size and location of tumour.
Other options include pneumonectomy (removal of the whole lung), wedge resection (removal of a small part of one of the lobes) or a sleeve resection (removing one lobe and part of the bronchi).
*Systemic mediastinal lymph node dissection should be performed during lung resection for primary lung cancer

Figure 8 – Lung cancer specimen following pneumonectomy
Lung function testing should be performed in all patients prior to resection, to calculate predicted post-operative respiratory capacity, which will guide the type of resection performed. Pneumonectomy and lobectomy will reduce FEV1 by 50% and 20% respectively, therefore pre-operative FEV1 target should be >1L for lobectomy and >2L for pneumonectomy.
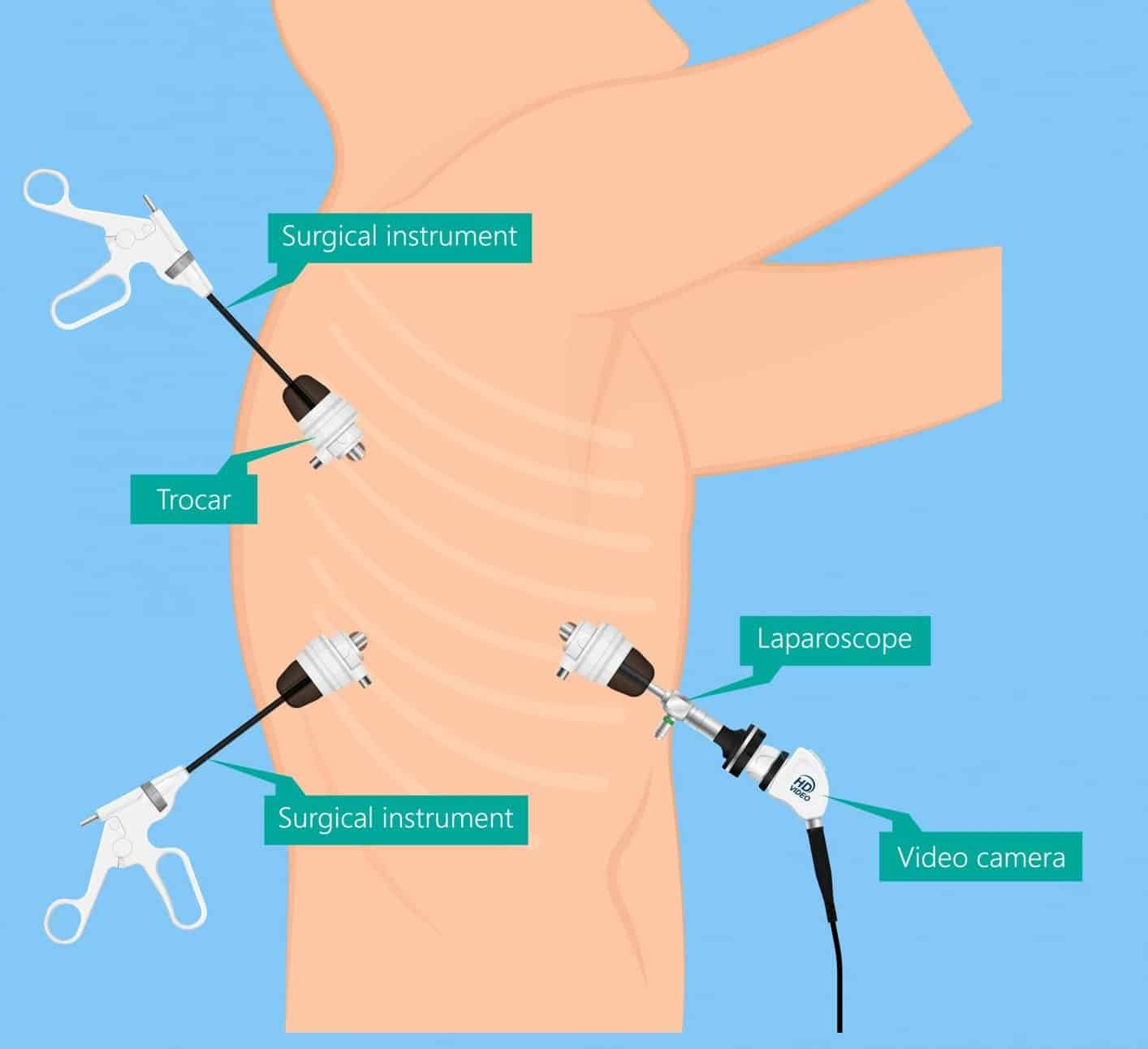
Video-Assisted Thoracoscopic Surgery
Video-assisted thoracoscopic surgery (VATS) lobectomy (Fig. 9) is widely becoming the standard approach for resection of early-stage lung cancer.
When compared to open techniques, VATS has been shown to have equivalent disease-free and overall survival outcomes, however VATS reduces post-operative pain, length of stay, fewer in-hospital complications, shorter hospital stay, preserved pulmonary function, and improved cosmetic result.
Complications
Prognosis of lung cancer unfortunately remains poor. Around 40% of people diagnosed with lung cancer survive for one year or longer, and 16% survive for five years or longer.
Key Points
- Lung cancer causes around 2 million deaths each year worldwide
- Common types of lung cancer include small cell carcinoma, squamous cell carcinoma, adenocarinoma, and large cell carcinoma
- Symptoms depend on type of lung cancer, location of primary tumour, and extent of any metastatic spread
- Definitive diagnosis comes from CT imaging and biopsy
- Surgical resection is the only definitive curative treatment options, however most patient unfortunately have metastatic disease at time of presentation