Introduction
Gallstone disease is a common condition, affecting around 10-14% in Western populations. Most individuals with gallstones will remain asymptomatic, however on average 1-4% of individuals will develop symptoms secondary to their gallstones.
Gallstones can cause a spectrum of disease, from biliary colic to acute pancreatitis, depending on the region of the biliary system involved. This article will focus on the presentation and management of biliary colic and acute cholecystitis.
Pathophysiology
Bile is formed from cholesterol, phospholipids, and bile pigments (products of haemoglobin metabolism). It is stored in the gallbladder, before passing into the duodenum upon gallbladder stimulation.
Gallstones form as a result of supersaturation of the bile. There are three main types of gallstones:
- Cholesterol stones – composed purely of cholesterol, from excess cholesterol production
- There is a well recognised link between poor diet, obesity, and cholesterol stones
- Pigment stones – composed purely of bile pigments, from excess bile pigments production
- Commonly seen in those with known haemolytic anaemia
- Mixed stones – comprised of both cholesterol and bile pigments
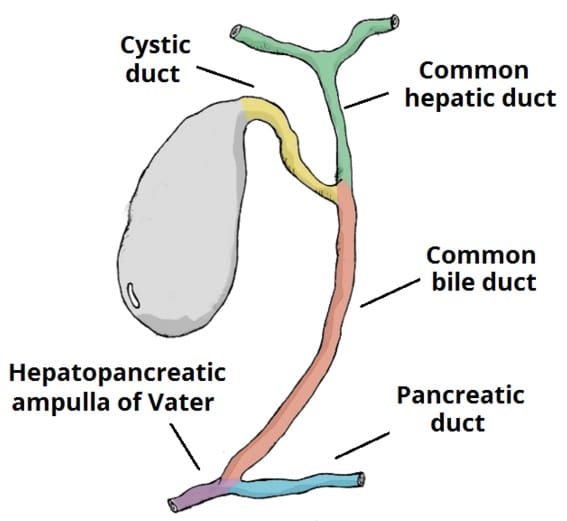
Figure 1 – The biliary system, which transports bile from the gallbladder to the duodenum
Risk Factors
Classically the common risk factors for gallstone disease are colloquially described as the “5 F’s”: Fat, Female, Fertile, Forty, and Family history.
Other recognised risk factors include pregnancy and oral contraceptives*, haemolytic anaemia (specifically for pigment stones), and malabsorption (such as previous ileal resection or Crohn’s disease).
*Oestrogen causes more cholesterol to be secreted into bile
Clinical Features
Studies have shown for those who are symptomatic, over 50% will present as biliary colic and 35% as an acute cholecystitis.

Figure 2 – Gallstone found incidentally on an ultrasound scan in an asymptomatic patient
Biliary Colic
Biliary colic occurs when the gallbladder neck becomes impacted by a gallstone. There is no inflammatory response, yet the contraction of the gallbladder against the occluded neck will result in pain.
The pain is typically sudden, dull, and colicky in nature. It is often focused in the right upper quadrant although it may radiate to the epigastrium and/or back. The pain may be precipitated by the consumption of fatty foods* and the patient often complains of nausea / vomiting. In general, once pain relief has been started, symptoms often settle quickly.
*Fatty acids stimulate the duodenum endocrine cells to release cholecystokinin (CCK), which in turn stimulates contraction of the gallbladder.
Acute Cholecystitis
Patients with acute cholecystitis will report a constant pain in the RUQ or epigastrium, associated with signs of inflammation, such as fever or lethargy.
Patients with acute cholecystitis will be tender in the RUQ and may demonstrate a positive Murphy’s sign. Ensure to check for any guarding (may suggest a gallbladder perforation) and for features of sepsis.
Murphy’s Sign
Whilst applying pressure in the RUQ, ask the patient to inspire. Murphy’s sign is positive when there is a halt in inspiration due to pain, indicating an inflamed gallbladder. This can be achieved more accurately with an ultrasound, namely the sonographic Murphy sign.
Differential Diagnosis
There are a wide variety of pathologies that can present with RUQ pain. However, differentials to consider include gastro-oesophageal reflux disease, peptic ulcer disease, acute pancreatitis, or inflammatory bowel disease.
Investigations
Laboratory Test
Certain blood tests can help in the initial evaluation of suspected cases:
- FBC and CRP – assess for the presence of any inflammatory response, which will be raised in cholecystitis
- LFTs – biliary colic and acute cholecystitis are likely to show a raised ALP (indicating ductal occlusion), yet ALT and bilirubin should remain within normal limits (unless a Mirizzi syndrome, discussed below)
- Amylase (or lipase) – to check for any evidence of pancreatitis
A urinalysis, including a pregnancy test if relevant, should be performed to exclude any renal or tubo-ovarian pathology.
Imaging
A trans-abdominal ultrasound (Fig. 2) is one of the most sensitive modalities for visualising gallstone disease and is typically used first line to investigate suspected gallstone pathology.
Three specific areas are often visualised on US:
- The presence of gallstones or sludge (the start of gallstone formation)
- Gallbladder wall thickness (if thick walled, then inflammation is likely)
- Bile duct dilatation (indicates a possible stone in the distal bile ducts)
If results from US scans are inconclusive, further imaging options are available. The gold standard investigation* for gallstones is Magnetic Resonance Cholangiopancreatography (MRCP), largely replacing ERCP for diagnostic purposes (Fig. 3). MRCP can show potential defects in the biliary tree caused by gallstone disease, with a sensitivity approaching 100%.
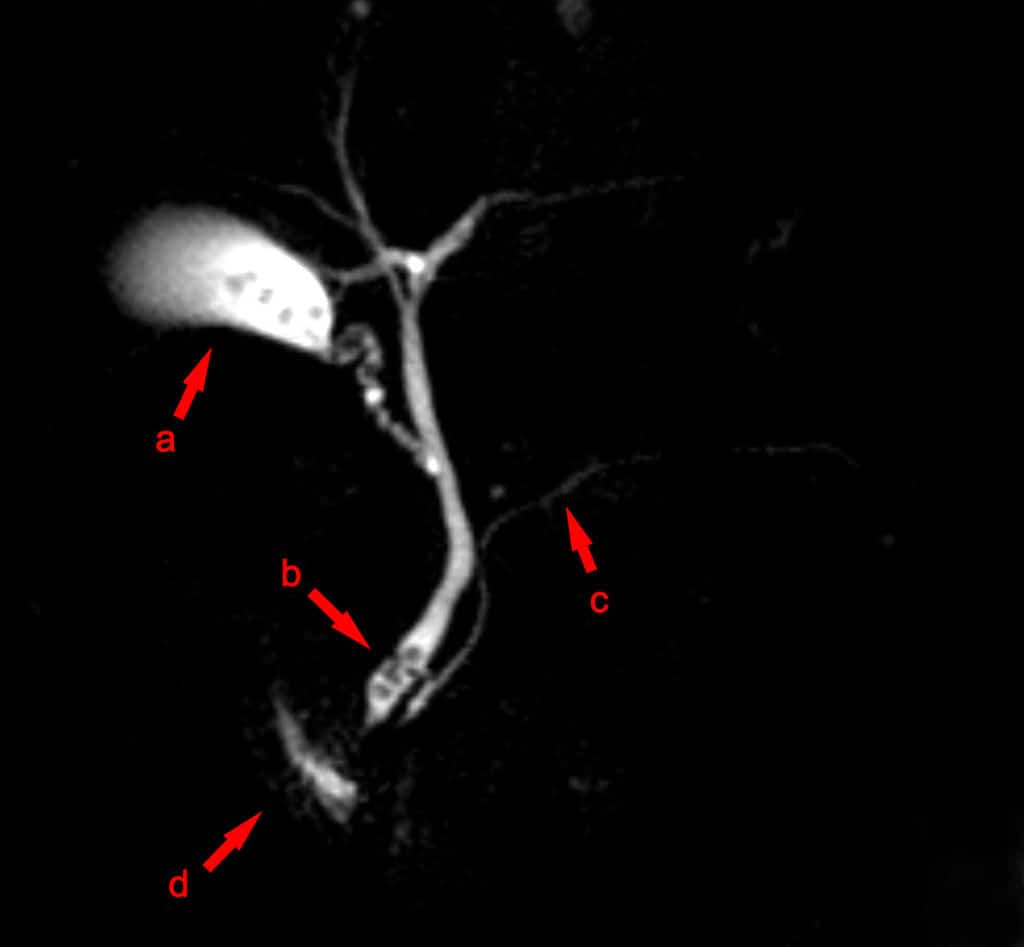
Figure 3 – MRCP image showing stones in the distal common bile duct: (a) Gallbladder with stones (b) Stone in bile duct (c) Pancreatic duct (d) Duodenum.
*Any patient with symptoms suggestive of gallstones with inconclusive US (or CT scans) should undergo a MRCP
Management
Biliary Colic
Patients with biliary colic should be prescribed analgesia (regular paracetamol +/- NSAIDs +/- opiates analgesia).
The patient should be advised about lifestyle factors that may help control symptoms (and help with future surgery), such as a low fat diet, weight loss, and increasing exercise.
Following first presentation of biliary colic, there is a high chance of symptom recurrence or the development of complications of gallstones, therefore an elective laparoscopic cholecystectomy* (Fig. 4) is warranted and should be offered within 6 weeks of first presentation.
*The laparoscopic route is preferred for cholecystectomy but is not always possible
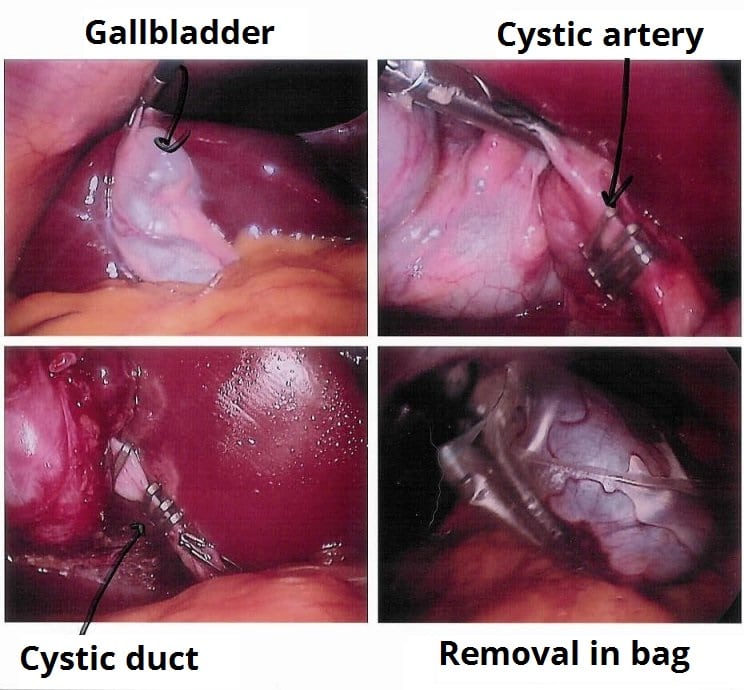
Figure 4 -Stages of a laparoscopic cholecystectomy
Acute Cholecystitis
Patients with acute cholecystitis should be started on appropriate intravenous antibiotics (such as co-amoxiclav +/- metronidazole). Concurrent analgesia and antiemetics should also be prescribed.
A laparoscopic cholecystectomy is indicated within 1 week of presentation, as per NICE guidance, however this ideally should be done within 72hrs of presentation for a likely simpler procedure*.
For those not fit for surgery and not responding to antibiotics, a percutaneous cholecystostomy can be performed to drain the infection (although as the gallstones remain in-situ, the risk of recurring disease remains).
*A Cochrane review previously demonstrated that earlier cholecystectomies are safe and reduce overall hospital stay
Any patient readmitted with RUQ pain post-cholecystectomy, it is important to exclude a retained CBD stone post-operatively. US abdomen scan may be useful, yet if this is unremarkable, then further investigation via MRCP imaging is warranted.
Complications
Mirizzi Syndrome
A stone located in Hartmanns pouch (an out-pouching of the gallbladder wall at the junction with the cystic duct) or in the cystic duct itself can cause compression on the adjacent common hepatic duct.
This results in an obstructive jaundice, even without stones being present within the lumen of the common hepatic or common bile ducts. Diagnosis is confirmed by MRCP and management is usually with laparoscopic cholecystectomy.

Figure 5 – Mirizzi syndrome causes by a stone lodged in Hartmann’s pouch, compressing the common hepatic duct
Gallbladder Empyema
A gallbladder empyema is when the gallbladder becomes filled with pus (Fig. 6). Patients will become unwell, often septic, presenting with a similar clinical picture to acute cholecystitis. They are associated with significant morbidity and mortality.
The condition is diagnosed by either US scan or CT scan. Treatment is via laparoscopic cholecystectomy* (may require intra-operative drainage if tense gallbladder) or percutaneous cholecystostomy (if unsuitable for surgery).
*There is a higher rate of conversion to open cholecystectomy with emypema than with uncomplicated acute cholecystitis
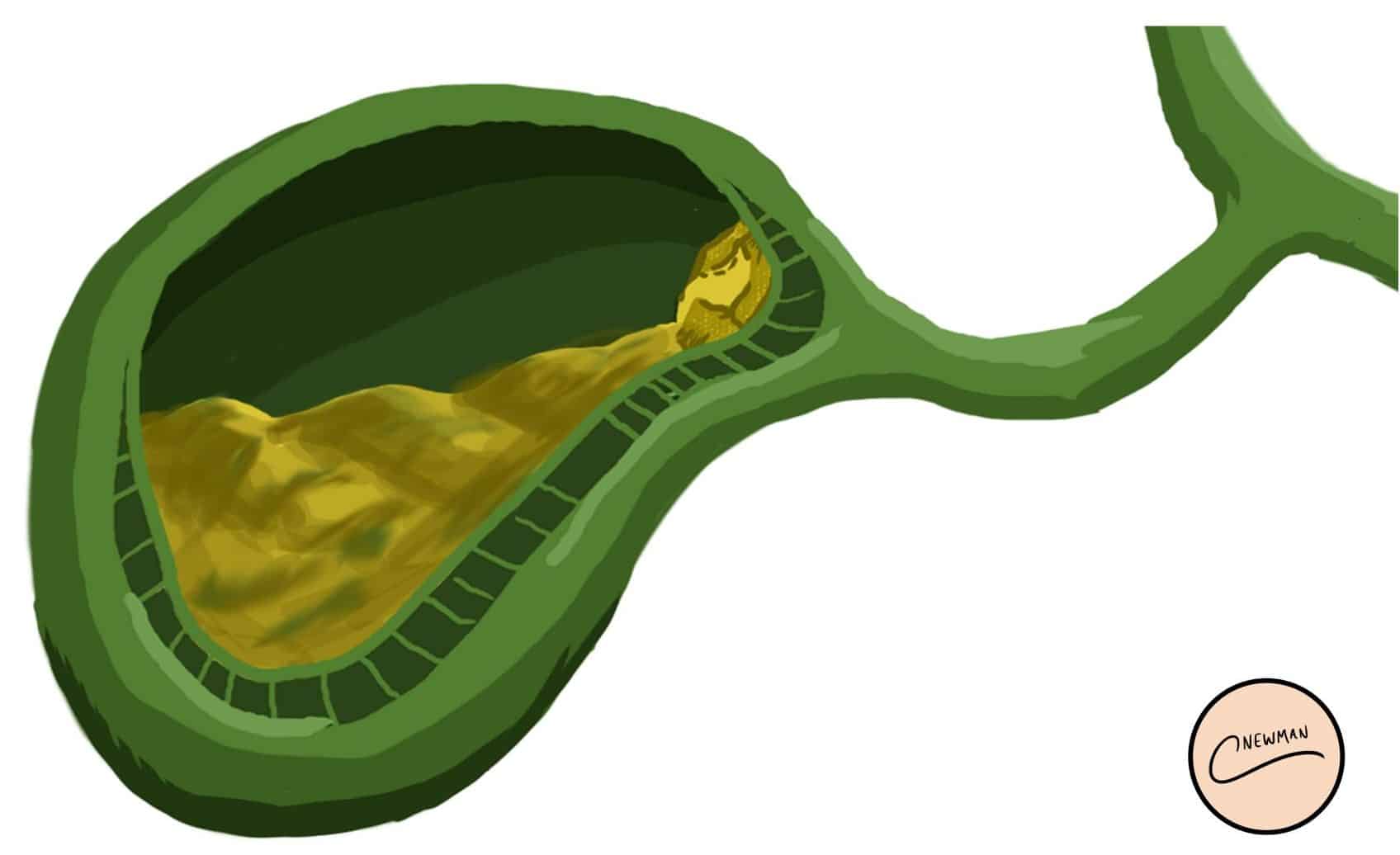
Figure 6 – Illustration demonstrating a gallbladder empyema
Chronic Cholecystitis
Patients with chronic cholecystitis will typically have a history of recurrent or untreated cholecystitis, which has led to a persistent inflammation of the gallbladder wall. Patients present with ongoing RUQ or epigastric pain with associated nausea and vomiting.
It can be diagnosed typically by CT imaging (or often noted on histology post-cholecystectomy). Management in uncomplicated cases is via elective cholecystectomy. Its main complications are gallbladder carcinoma and biliary-enteric fistula.
Bouveret’s Syndrome and Gallstone Ileus
Inflammation of the gallbladder (typically if recurrent) can cause a fistula to form between the gallbladder wall and the small bowel (Fig. 7), termed a cholecystoduodenal fistula, allowing gallstones to pass directly into the small bowel (typically at the duodenum)
As a consequence, bowel obstruction can occur:
- Bouveret’s Syndrome – a stone impacts in the proximal duodenum, causing a gastric outlet obstruction
- Gallstone Ileus*– a stone impacts at the terminal ileum (the narrowest part of the small bowel), causing a small bowel obstruction
*The term ileus is misleading, as it is actually a bowel obstruction
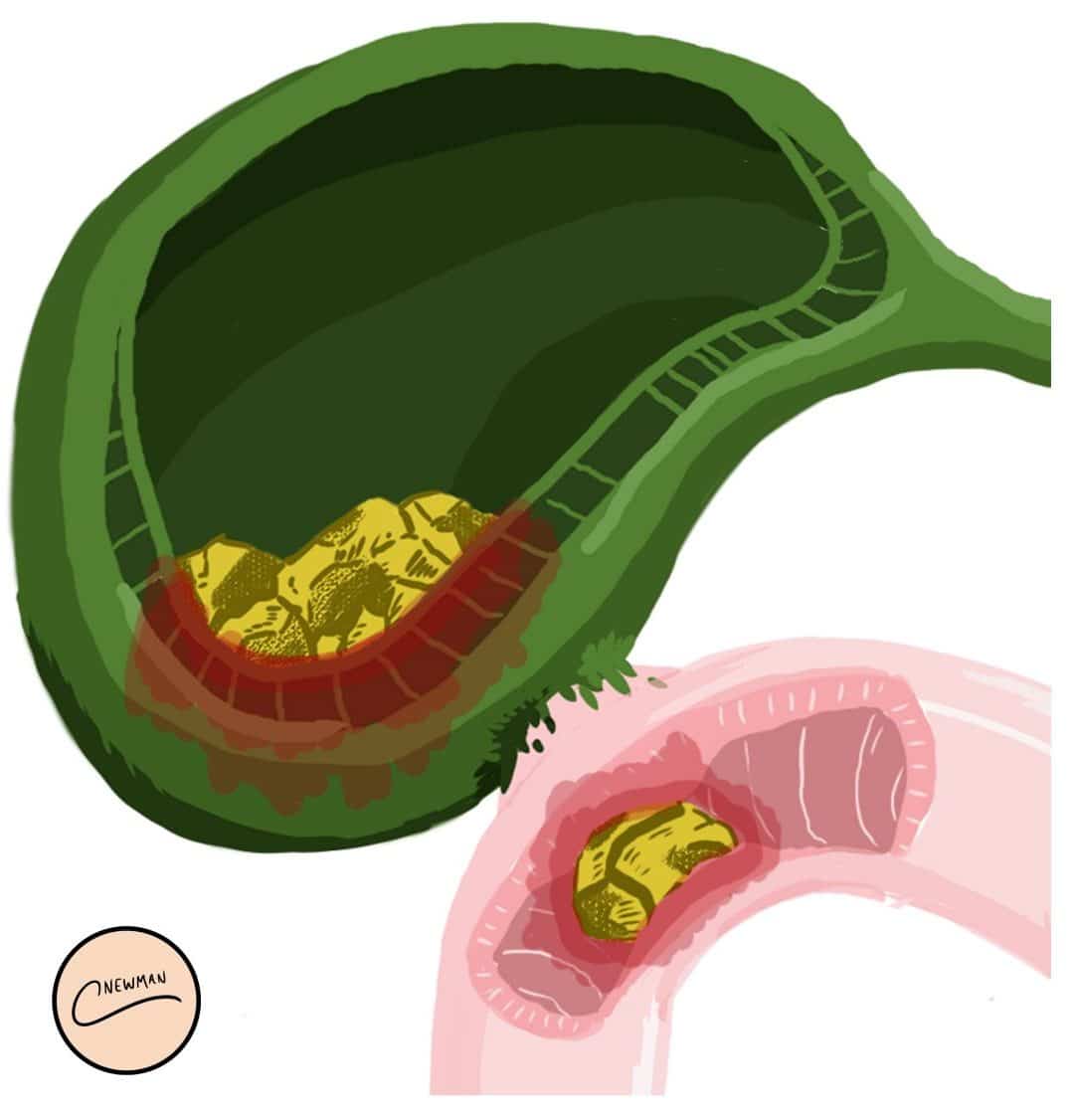
Figure 7 – A Cholecystoduodenal Fistula, resulting in a gallstone entering the small bowel
Key Points
- Gallstones are a very common condition, either symptomatic or asymptomatic
- Risk factors include high-fat diet, female gender, malabsorption, and oral contraceptive use
- Most cases can be diagnosed by US abdomen scan
- Definitive treatment for simple gallstone disease is via laparoscopic cholecystectomy
