Introduction
Osteoarthritis (OA) is a degenerative joint disease, characterised by the loss of articular cartilage. This is associated with periarticular bone response, the features of which can be seen on plain film radiographs.
OA is extremely common, with prevalence increasing with age. It is the most common cause of disability for older adults in developed countries. The most commonly affected joint is the knee joint, followed by the hip joint.
In this article, we shall look at the risk factors, clinical features, and management of knee osteoarthritis.
Risk Factors
- Genetic factors – Estimates suggest a genetic component for hand, knee and hip OA at around 40-60%, however the specific genes involved remain largely unknown
- Constitutional factors – Factors including increasing age, female gender, obesity, and low bone density (specifically in the progression of OA)
- Local factors – Previous joint injury, occupational or recreational stresses on the joint, reduced surrounding muscle strength, or any joint laxity or malalignment
Clinical Features
The most common feature of knee OA is pain. Pain is typically felt around the knee, however can radiate to the thigh and hip. This pain is usually exacerbated by exercise and relieved by rest.
Patients will often have bilateral disease. There is associated joint stiffness, which can result in reduced function, and even joint swelling in severe cases.
On examination, there will be a reduced range of movement and often evidence of muscle wasting. Crepitus can be felt in severe cases.
Differential Diagnosis
The main differentials to consider is a patient presenting with joint pain and stiffness includes any meniscal or ligament injury, referred pain from another joint or the back, crystal arthropathies, or patellofemoral arthritis (see below).
Investigations
Most cases of OA can be investigated with a plain film radiograph alone (lateral and antero-posterior (AP) views). The diagnostic features* (Fig. 2) that can be seen are (mnemonic LOSS):
- Loss of joint space
- Osteophytes
- Subchondral sclerosis
- Subchondral cysts
Further views, such as a skyline view of the knee, can be useful to further assess for any patellar involvement (see below).
Additional investigations are only required when alternative differentials are suspected, such as blood tests for any infective cause or MRI imaging in ligamentous injury.
*Only one or two of these markers may be present; osteophyte formation tends to be evident only in later stages of the disease

Figure 2 – Left knee OA, demonstrating extensive osteophytes, narrowing of the joint space (arrow), and increased subchondral bone density
Classification
The Kellgren and Lawrence system can be used to classify the severity of knee OA:
- Grade 0 – no radiographic features of OA are present
- Grade 1 – unclear joint space narrowing and possible osteophytic lipping
- Grade 2 – definite osteophytes and possible joint space narrowing on AP weight-bearing views
- Grade 3 – multiple osteophytes, definite joint space narrowing, evidence of sclerosis, and possible bony deformity
- Grade 4 – large osteophytes, marked joint space narrowing, severe sclerosis, and definite bony deformity
Management
Initial Management
Lifestyle modifications play an essential part of the management plan, including weight loss, regular exercise, and smoking cessation. Adequate pain control is important, using the WHO analgesic ladder, to ensure ongoing mobility and quality of life.
Physiotherapy is commonly used and should be provided for all individuals with OA, aiming to slow disease progression and improve joint mechanics.
If conservative management efforts do not work, surgical management is warranted, which is typically either total or partial knee replacement.
Surgical Management
Total knee replacement (TKR) is the standard treatment for advanced osteoarthritis (Fig. 3). During this procedure, plastic and metal inserts are used to replace bone and cartilage in all sections of the knee. The vast majority of total knee replacements will function for at least 10 years and the majority of patients experience a significant reduction in knee pain.
Around 10% of patients only require partial (unicondylar) knee replacement, which is mainly used for those with disease localised to either the medial or lateral compartment, meaning the affected compartment will be replaced and healthy compartment left intact. Partial knee replacements are more conservative, therefore have faster recovery times, but may need conversion to total knee replacement at a later date.
Patellofemoral Osteoarthritis
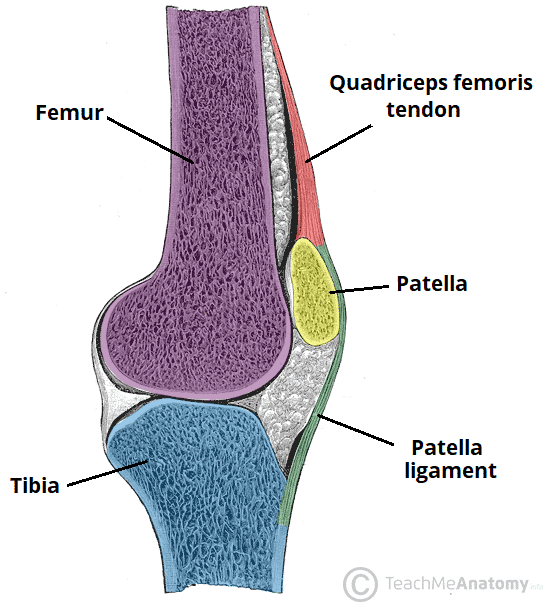
The patella rests in a groove on top of the femur called the trochlear groove, such that when the knee flexes and extends, the patella moves back and forth inside this groove.
Patellofemoral OA is osteoarthritis affecting the articular cartilage along the trochlear groove and on the underside of the patella.
Risk factors for the condition include patella dysplasia (resulting in the patella not fitting properly in the trochlear groove) or previous patella fracture (leading to damage to the articular cartilage).
Clinical Features
Anterior knee pain is the most common presenting symptom for patellofemoral OA, however specifically is worse with activities that put pressure on the patella, such as climbing a flight of stairs.
It can be associated with joint stiffness and swelling. Diagnosis is mainly made from the history, then confirmed with plain film radiographs (specifically with the skyline view, Fig. 4).
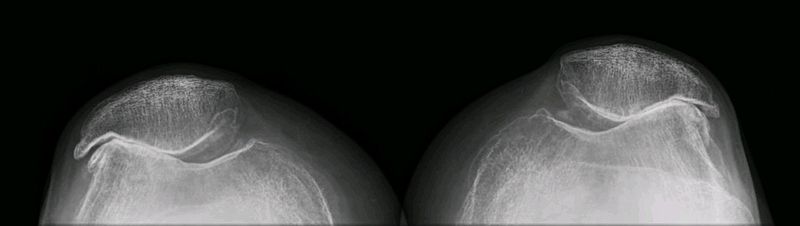
Figure 3 – Severe bilateral patellofemoral osteoarthritis
Management
Initial management is conservative, much the same as for knee OA. In unsuccessful cases however, patellofemoral replacement may be required, however this cannot be carried out if there is OA involving other parts of the knee, which instead would warrant a total knee replacement.
Key Points
- The knee joint is the most commonly affected joint by osteoarthritis
- The most common feature of knee osteoarthritis is pain, exacerbated by exercise and relieved by rest
- Most cases of osteoarthritis can be investigated with a plain film radiograph alone
- Initial management is with analgesia and physiotherapy, however total knee replacement (TKR) is the standard treatment for advanced osteoarthritis