Introduction
The number of heart and lung transplants has increased over recent years, due to a combination of better surgical techniques and patient management pre- and post-operatively. However, there remains a significant shortage of appropriate organs, resulting in considerable waiting lists and subsequent mortality among patients waiting for a transplant.
Bridges to transplantation are used to manage patients who are listed for a heart or lung transplant, acting to temporise whilst on the waiting list. Various approaches are used, depending on the underlying diagnosis and patient characteristics.
The main two classifications are ventricular assist devices (VAD) and extracorporeal membrane oxygenation (ECMO). VADs only provide circulatory support, whereas ECMO oxygenates the blood too.
Ventricular Assist Devices
A VAD is a mechanical pump that provides adequate cardiac output to perfuse end-organs, while unloading the heart.
The key components of a VAD are an inflow cannula (implanted in the ventricle), a pumping chamber, an outflow cannula (implanted into the aorta or pulmonary artery), and a drive line (extracorporeal control and power lines that extend from pumping chamber to outside the body).
VADs are commonly implanted in the left ventricle, but can be implanted in the right ventricle, or both. The VAD circuit receives blood from the heart and pumps into the arterial circulation. The VAD circuit runs parallel to the native cardiac circuit, but the ventricle functions as a passive conduit mainly due to poor contractility.
Indications for VAD
Indications for a VAD vary depending on the patient, however the most common are severe symptomatic heart failure, intractable arrhythmias, or advanced heart failure complicated by cardiac cachexia or renal/hepatic failure (not responsive to medical therapy).
As such, the three major clinical scenarios its used are as a bridge to transplantation (whilst on the waiting list), as destination therapy (patients who are not transplant candidates or who decline transplantation), or as a bridge to recovery (those with reversible cardiac dysfunction).
Types of Ventricular Assist Devices
VADs are classified based on the side of the heart that is assisted, the type of pump used, and whether the device is internal or external.
Those classified by the side of the heart being assisted include:
- Left ventricular assist device (LVAD) receives inflow from the left atrium or left ventricle and outflows into the aorta (Fig. 1)
- Right ventricular assist device (RVAD) receives inflow from the right atrium or right ventricle and outflow into the pulmonary artery
- Biventricular assist device (BiVAD) consists of an LVAD and RVAD attached in parallel (or as a dual chamber device which is known as a total artificial heart (TAH))
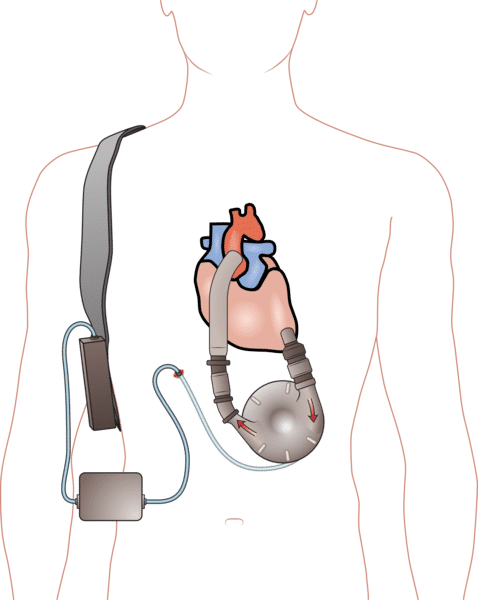
Figure 1 – Schematic demonstrating an intracorporeal left ventricular assist device (LVAD)
VADS can be pulsatile or non-pulsatile; pulsatile VADs mimic the natural action of the cardiac ejection cycle, whilst non-pulsatile VADs use a motor at fixed speeds which maintains a constant ejection of blood into the systemic circulation*
VADs can also be classified as either intracorporeal (implantable) or extracorporeal (external); intracorporeal VADs have the pump below the heart within the thoracic cavity and power source outside the body (Fig. 1), whilst extracorporeal VADs have the pump and power source outside the body
*This means patients with a non-pulsatile VADs often lack a pulse on palpation
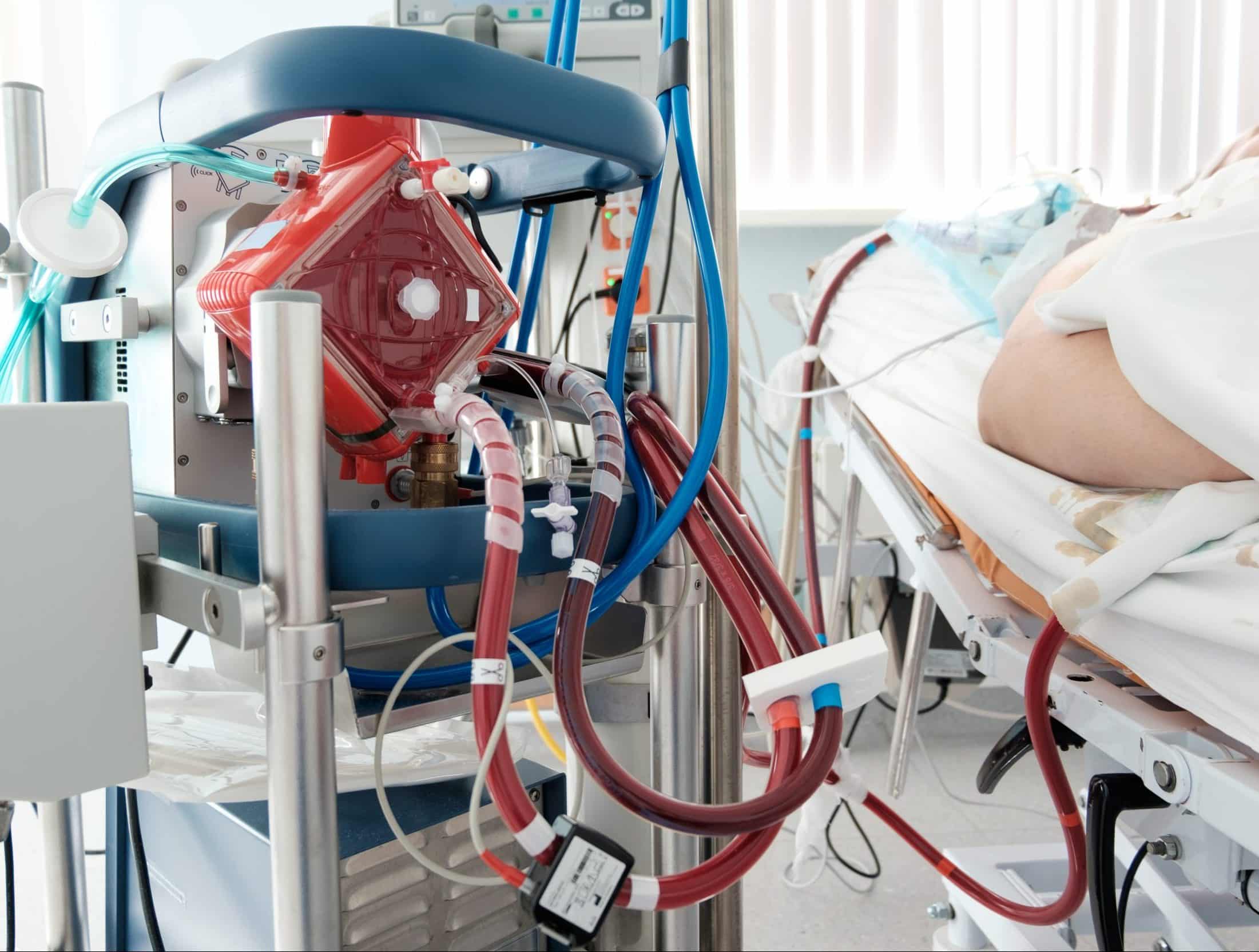
Extracorporeal Membrane Oxygenation
Extracorporeal membrane oxygenation (ECMO) is used to provide prolonged cardiac and respiratory support to patients whose heart and lungs are unable to sustain adequate perfusion.
ECMO is similar in principle to cardiopulmonary bypass and contains similar components, but there are several key modifications that enable ECMO support to continue for days rather than hours.
The ECMO machine is connected to the patient via cannulas inserted through the groin, axilla, or neck (especially in neonates and infants). The blood is pumped from the patient’s body to an oxygenator that adds oxygen and removes carbon dioxide, therefore replacing the lung function. The ECMO machine then sends the blood back to the patient via a pump with the same force as the heart, therefore replacing the heart function.
Indications for ECMO
Indications for ECMO include acute heart failure (such as secondary to MI or drug toxicity), primary graft failure following cardiac or lung transplantation, massive pulmonary embolism, or acute respiratory distress syndrome
Types of ECMO
There are two main types of ECMO:
- Venovenous – venous blood is accessed from large central veins, typically femoral, pumped through the oxygenator, and returned to the venous system near right atrium
- This provides respiratory support only
- Venoarterial – venous cannula is typically inserted into the common femoral vein and an arterial cannula is inserted into the femoral artery, which is used to pump the blood back into the patient
- This provides both respiratory and haemodynamic support
Key Points
- Bridges to transplantation are used to manage patients who are listed for a heart or lung transplant, acting to temporise whilst on the waiting list
- The main two classifications are ventricular assist devices (VAD) and extracorporeal membrane oxygenation (ECMO)
- Most common indications for a VAD are severe symptomatic heart failure, intractable arrhythmias, or advanced heart failure complicated by cardiac cachexia or renal/hepatic failure
- Most common indications for ECMO include acute heart failure, primary graft failure following cardiac or lung transplantation, massive pulmonary embolism, or acute respiratory distress syndrome