Introduction
Septic arthritis refers to the infection of a joint. It requires a high index of suspicion and can affect both native and prosthetic joints.
The main causative organisms that lead to septic arthritis are S. aureus (most common in adults), Streptococcus spp., Gonorrhoea (more common in sexually active patients), and Salmonella (especially in those with sickle cell disease).
Bacteria will ‘seed’ to the joint from a bacteraemia (e.g. recent cellulitis, UTI, chest infection), a direct inoculation, or spreading from adjacent osteomyelitis. Septic arthritis can cause irreversible articular cartilage damage leading to severe osteoarthritis.
In this article, we look at the risk factors, clinical features and management of septic arthritis.
Risk Factors
The main risk factors for developing septic arthritis are increasing age, any pre-existing joint disease (e.g. rheumatoid arthritis), diabetes mellitus or immunosuppression, chronic kidney disease, hip or knee joint prosthesis, or intravenous drug use
Clinical Features
Patients will most commonly present with a single swollen joint causing severe pain. Pyrexia will be in around 60% of affected individuals (although its absence should not rule out septic arthritis). The joint is often fixed in the position of maximum volume.
On examination, the joint will appear red, swollen, and warm, causing pain on active and passive movements. An effusion may also be evident.
Often the joint is rigid and the patient will not tolerate any passive movement at all, and will be unable to weight bear. Symptoms are more florid and obvious in native joint injection; in prosthetic joint infections, the features can be more subtle.
Differential Diagnoses
Septic arthritis should be the main differential diagnosis in anyone presenting with a single painful swollen joint. However, other differentials to consider are worsening osteoarthritis, haemarthrosis, crystal arthropathies such as gout and pseudogout, rheumatoid arthritis, reactive arthritis, or Lyme disease (infection with Borrelia burgdoferi)
Septic Arthritis in Children
Septic arthritis can occur in any age but it is important to consider in the differential for a warm and swollen joint in paediatrics. Additional differentials in children to consider are transient synovitis, osteomyelitis, and juvenile idiopathic arthritis.
The Kocher criteria can be used to differentiate between septic arthritis and transient synovitis in a child with a painful hip. The components of the criteria are being unable to weight-bear, pyrexial, and having an elevated White Cell Count (WCC) and elevated Erythrocyte Sedimentation Rate (ESR)
Each component is given a score of 0 or 1 depending on the features; a score of 3 or more gives a 93% probability of septic arthritis. The investigation and management is similar to adults, requiring irrigation and washout of the affected joint and concurrent antimicrobial therapy
Investigations
Routine bloods including FBC and CRP, should be sent, alongside ESR and urate levels. Blood cultures should also be sent (at least two separate samples), especially in those with evidence of sepsis.
A joint aspiration is essential and should also be performed before antibiotics are given (if practicable and safe to do so); for those involving a prosthetic joint, this should only be done in the operating room. Joint fluid analysis should also be sent for Gram stain (Fig. 2), leucocyte count, polarising microscopy, and fluid culture.
It is important that cultures and joint aspiration are sent where possible prior to starting antibiotics (unless the patient is overtly septic).
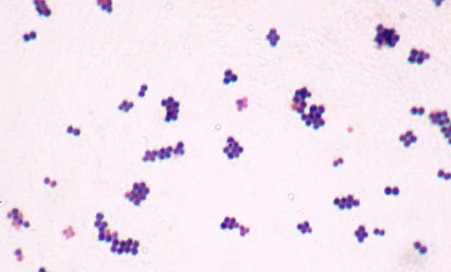
Figure 2 – S. Aureus, as seen on Gram stain
Imaging
A plain radiograph of the affected joint is often performed; whilst in early stages, no evidence of the disease may be present, it may eventually progress to demonstrate capsule and soft tissue swelling, fat pad shift, or joint space widening.
Further imaging is rarely performed*. Ultrasound imaging can be useful to guide joint aspiration and for drainage (particularly for the hip), whilst CT/MRI imaging is a very sensitive method in assessing joint damage, typically used if there is an uncertainty in the diagnosis.
CT or MRI imaging may also be useful in specific joint infections (such as the sternoclavicular or sacroiliac) to assess any extension into the mediastinum or pelvis. Radionuclide scans can be useful in identifying septic arthritis in isolated joints, such as the sacroiliac joint.
Management
Any septic patient should be managed appropriately, with early resuscitation and investigation as a priority.
Empirical antibiotic treatment should be started as soon as possible, after any planned cultures and aspirates have been performed. This should be switched to culture directed antibiotic therapy as soon as results are available. As a guide, antibiotics are typically administered for long term (around 4-6 weeks), initially intravenously (around 2 weeks).
Infected native joints are a surgical emergency and require surgical irrigation and debridement (‘washout’) in theatre to aid source control, with irreversible cartilage damage ocurring within 8 hours of infection. This may be needed a number of times before the infection has cleared.
If the infection is within a prosthetic joint, washout is still required, but revision surgery (either acutely or staged) is typically needed.
Complications
The main complications of septic arthritis are osteoarthritis and osteomyelitis. Early intervention will reduce the risk of developing these complications.
Key Points
- Septic arthritis is infection of a joint and is an orthopaedic emergency
- Patients present with acute painful, swollen, and tender joints, and importantly are unable to weight bear or passively move
- Blood cultures and joint aspiration is essential, prior to any antibiotic management if possible
- Patients are at increased risk of developing osteoarthritis and osteomyelitis


