Introduction
Foreign bodies (FBs) in the ear, nose, or throat are extremely common emergency presentations to ENT teams.
Foreign bodies in the ear or nose are more common in children, people with learning difficulties, or those with psychiatric disorders. Oesophageal soft foreign bodies are seen in older people or in patients with oesophageal disorders.
Whilst ear FBs do not tend to cause serious complications, aspirated or ingested FBs can lead to life-threatening airway compromise or oesophageal perforation if left unmanaged.
Clinical Features
The approach taken for a FB will depend on where the suspected foreign body is located. From the history, it is important to clarify the nature of the object*, the timing of ingestion or insertion, and any previous history of FB insertion.
- For ear foreign bodies, ask about any pain or discharge from the ear, and any associated hearing loss
- For nose foreign bodies, ask about issues with breathing and about any nasal discharge
- For ingested foreign bodies, clarify specifically the nature of the object, whether sharp (e.g. a fish bone) or soft (e.g. cooked meat); check for any dysphagia, including if the patient is able to swallow saliva
*Organic materials (e.g. food or live objects) need to be removed more urgently than non-organic materials (e.g. plastic), as organic materials can cause tissue oedema and swelling, making it more difficult to remove with time; any live insects in the ear should be drowned in oil;
Examination will be dependent on where the suspected foreign body is located. For the ear, direct visualisation of the FB is usually possible with otoscopy, whilst for the nose, use an age-appropriate Thudicum speculum (size 0 or 1 for children, 2 or 3 for adults) and a head-torch or otoscope is usually required.
For FB in the pharynx, visual examination of oropharynx can be attempted using a Lack’s tongue depressor and head-torch. Palpate for points of tenderness on the neck (and assess whether this moves on swallowing), as well as for surgical emphysema. A flexible nasal endoscopy (FNE) is usually required as an adjunct for examination to visualise the pharynx, especially if not visible on initial assessment.
Red Flags for Foreign Bodies
The important red flags for any patient presenting with a foreign body include:
- Any signs of airway compromise, such as stridor, dysphonia, or drooling
- Any signs of oesophageal perforation, such as chest pain, back pain (mediastinitis), features of sepsis, or surgical emphysema
- Any history of button battery ingestion
Differential Diagnosis
There will usually be a clear history of foreign body ingestion, but the top differential for a suspected ingested FB is a food bolus, particularly if the patient is unsure whether they ate anything with bones.
Occasionally, patients presenting with ear infections (particularly otitis externa) for several weeks may have placed a foreign body in the ear and may be unaware of it – cotton buds are common culprits.
Insidious unilateral nasal discharge may be due to a foreign body, however if this occurs in an older patient, malignancy must be considered.
Investigations
No further investigations are usually required for nose and ear FBs.
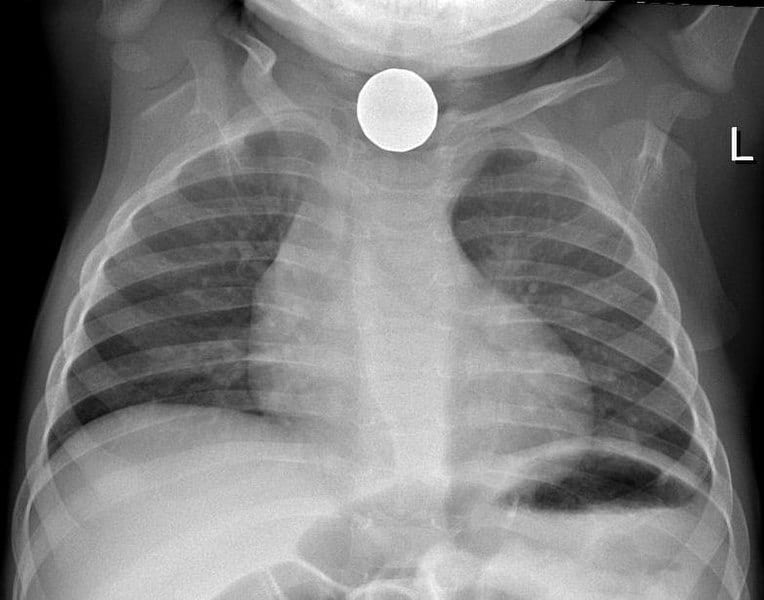
If there is a moderate clinical suspicion of an ingested foreign body, initially a plain film radiograph lateral soft-tissue neck can be performed, however this has poor sensitivity (around 57%) and specificity (around 76%).
Plain film radiographs can be used to assess for the foreign body (if radio-opaque), the presence of surgical emphysema, any widening of retropharyngeal tissue (approximate measurements are >7mm at C2, >22mm at C7), or loss of cervical lordosis
If plain films do not show anything, however clinical suspicion remains, a CT neck can be performed to further assess the area (sensitivity near 100%). Additionally, a plain film chest radiograph (CXR) can be performed to assess for any mediastinal widening, which is a red flag sign.
Management
The urgency of FB removal depends entirely on the location and nature of the FB, and the patient’s clinical status. An A to E approach should always be employed on initial assessment. For an ingested FB, if there are any signs of airway compromise, proceed as for a patient with stridor.
Button batteries can erode and cause irreversible caustic burns, therefore any button battery ingested must be removed immediately.
Ears
Ear foreign bodies can be removed using an array of instrumentation, such as microsuction with a Zoelner sucker, crocodile forceps, Jobson-Horne probes, or wax hooks
If the FB is medial against the tympanic membrane or simply it cannot be removed, patients can be safely discharged home with a view to removing the foreign body under general anaesthesia (unless a button battery in which case immediate removal is needed), whilst organic materials will often need urgent removal.
Nose
Nose FB management is similar to that for ear FB, however emergency removal under GA should be performed if the patient is distressed or any signs of breathing difficulty.
If unable to remove or unsure if the FB is present, consent and work-up for examination under anaesthesia and removal.
Throat
If the FB is visualised in the oropharynx and the patient can tolerate the procedure, removal may be attempted using Magill forceps and laryngoscope, with adequate local anaesthetic.
Flexible nasendoscopy can be used to aid visualisation of the oropharynx whilst removing the foreign body. Otherwise, removal should be attempted with endoscopy under general anaesthesia (either via pharyngoscopy / laryngoscopy or rigid oesophagoscopy).
The urgency of endoscopy is outlined below:
- Emergency endoscopy
- Any red flag signs
- Any sharp or long (>5cm) object in the oesophagus
- Urgent endoscopy (within 24 hours)
- Oesophageal obstruction (unable to swallow saliva)
- Blunt oesophageal FB
- Magnets proximal to the duodenum
- Non-urgent endoscopy
- Disc or cylindrical batteries which have passed into stomach without signs of injury
- Coins may be observed for up to 24 hours before removal if asymptomatic

Figure 2 – Foreign Body in the Oesophagus, as seen on Upper GI Endoscopy
Follow-up
After successful removal of nasal or ear FBs, patients can usually be discharged without follow up.
Any adult presenting with unilateral symptoms (e.g. hearing loss, nasal discharge) which persists after FB removal should raise suspicions of a head and neck cancer, therefore consider an urgent follow-up for these patients.
Patients with tympanic membrane perforation can be followed up routinely afterwards in primary care to ensure it has healed; if not, they can be referred routinely to ENT with advice on ear hygiene (to keep ear dry, avoid cotton bud use).
Patients who have undergone rigid oesophagoscopy should undergo a period of observation afterwards to ensure resolution of symptoms and monitoring for signs of perforation. Sterile water can then be introduced, before building up to a soft diet prior to discharge.
Food Bolus
Soft food boluses are also common presentations, however the clinical approach is similar to a suspected ingested foreign body.
On assessment, if there is any suspicion of sharp foreign body ingestion (e.g. bones) or any red flag signs, then manage as for an ingested FB. If the patient is unable to swallow their saliva, this is often a serious sign.
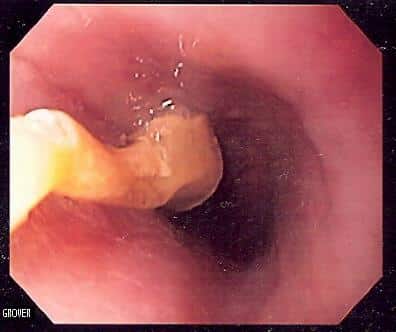
Figure 3 – Upper GI endoscopy showing an oesophageal food bolus obstruction due to a grape
Food bolus are found more in those with pre-existing oesophageal dysmotility or strictures. If there is a recurrent history of food bolus obstruction, the patient will need investigation for an underlying malignancy or other cause.
Otherwise, the patient can usually be observed for a period to assess for resolution of symptoms with medical management as below. If there is no resolution, an urgent upper GI endoscopy should be arranged.
Several medical therapies are often trialled (although evidence is lacking for their efficacy against observation alone), such as:
- Carbonated drinks (e.g. coke or lemonade)
- Glucagon 1-2mg IV
- Hyoscine butylbromide (Buscopan) 20mg IV
- Prokinetics, such as metoclopramide or erythromycin
- Diazepam 10mg IV
After resolution of symptoms, the patient should be observed and discharged if tolerating oral fluids and soft diet.
Key Points
- Foreign body insertion is a common presentation to emergency departments
- Red flag signs include evidence of airway compromise, of oesophageal perforation, or any button battery ingestion
- The urgency of FB removal depends entirely on the location and nature of the FB, and the patient’s clinical status
- Soft food boluses are also common presentations, however the clinical approach is similar to a suspected ingested foreign body