Introduction
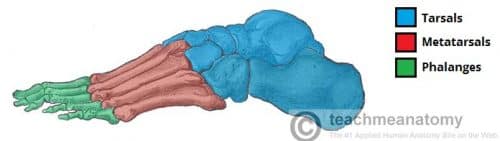
Hallux valgus (also commonly termed a “bunion”) is a deformity at the first metatarsophalangeal joint (MTPJ).
It is characterised by medial deviation of the first metatarsal and lateral deviation +/- rotation of the hallux, with associated joint subluxation.
This condition is one of the most common foot problems in the adult population, with a prevalence of around 35% in those aged >65yrs and more common in women.
In this article, we shall look at the pathophysiology, clinical features and management of hallux valgus.
Pathophysiology
During the gait cycle, the digits should remain parallel to the long axis of the foot. This is made possible by a balance between static stabilisers (bones and ligaments) and dynamic stabilisers (muscles and tendons). Due to the gross anatomy of the foot, the first metatarsal remains inherently unstable, heavily relying on these stabilising structures. There is therefore a greater risk of disturbing the fine balance.
Once the metatarsal head escapes the intrinsic anatomical control, the extrinsic tendons become a deforming force, causing the first metatarsal head to drift medially. This medial joint tension causes the bone to proliferate on the dorsomedial aspect of the head of the first metatarsal and the cartilage is affected by the subsequent remodelling.
Anatomical variants, genetic predisposition, and environmental factors can all further contribute. In predisposed individuals, wearing high-heels or narrow-fitting footwear can aggravate the condition by keeping the hallux in a valgus position.
Risk Factors
The main risk factors for developing hallux valgus include female gender, connective tissue disorders, and hypermobility syndromes. Anatomical variants that predispose to the condition include a long first metatarsal bone, malalignment of the first MTP joint, and flat feet.
Clinical Features
Hallux valgus typically presents with a painful medial prominence, likely aggravated by walking, weight-bearing activities, or wearing narrow toed shoes. Symptoms have often been present for some time before presentation, however have worsened in frequency and intensity
On examination, assess position and lateral deviation of the hallux (Fig. 2) and check for evidence of inflammation or skin breakdown over the prominence at the base of the hallux. Check for worsening of the prominence in the weight-bearing position.
Examine the foot in both a non-weight-bearing position and weight-bearing position.

Figure 2 – Right Hallux Valgus
Assess range of movement* (active and passive) and crepitus, as the presence of associated pain and crepitation is indicative of cartilage degeneration
Contracture of the extensor hallucis longus tendon may be visible in longstanding joint subluxation and any excessive keratosis on the foot may indicate signs of abnormal weight distribution from an altered gait.
*A normal range of movement is 5mm in both the dorsal and plantar direction from neutral, with no motion detectable in the transverse plane (this may be present to some degree in hallux valgus)
Differential Diagnoses
Differentials to consider for patients with hallux valgux include gout, septic arthritis, hallux rigidus, osteoarthritis, and rheumatoid arthritis
Investigations
The main investigation is plain film radiographs (Fig. 3), used to assess hallux valgus; it is often useful for the degree of lateral deviation and signs of joint subluxation.
This is measured as the angle between the first metatarsal and the first proximal phalanx; hallux valgus is diagnosed if the angle to be corrected is greater than 15 degrees (mild 15-20°, moderate 21–39°, and severe >40°)
Management
All patients should be prescribed sufficient analgesia, limiting the effects of the condition on quality of life.
Advise on adjusting footwear to prevent the deformity from worsening and preventing irritation of the skin over the medial eminence. If the patient has flat feet, then an orthosis may help to prevent the progression of the condition.
Physiotherapy can provide stretching exercises and gait re-education as indicated.
Surgical Management
Patients with a significantly impacted quality of life by the condition can be considered for surgical intervention, for which there are a variety of procedures possible:
- Chevron procedure – a ‘V shaped’ osteotomy of the distal first metatarsal is created, allowing the first metatarsal to be shifted laterally back into a normal alignment, then fixed by pins and screws
- Commonly used for mild deformities
- Scarf procedure – a longitudinal osteotomy is made within the shaft of the first metatarsal, for the distal portion to be moved laterally and fixed with two screws
- Useful for when the deformity is moderate to severe
- Lapidus procedure – the base of the first metatarsal and medial cuneiform are fused
- Often used when the underlying cause is tarsometatarsal joint hypermobility
- Keller procedure – an incision is made over the first MTPJ and the joint capsule is opened to expose the joint, with the diseased joint surfaces removed for a space to be left that is stabilised by suturing of surrounding tissues and subsequent scar tissue
- Commonly chosen when the first MTPJ arthritis is severe
Complications
Complications of hallux valgus include avascular necrosis, non-union, displacement and reduced range of movement.
Prognosis is variable in this condition as the deformity may remain stable or progress rapidly. Conservative management can help to alleviate symptoms but will never correct the deformity.
Key Points
- Hallux valgus is a deformity at the first metatarsophalangeal joint, characterised by medial deviation of the first metatarsal and lateral deviation +/- rotation of the hallux
- Patients will present with a painful medial prominence, likely aggravated by walking and weight-bearing
- Radiographic is often useful to assess degree of severity
- Management is conservative initially however several surgical options are available for those suitable for intervention