Introduction
Pilonidal sinus disease is a disease of the inter-gluteal region*, characterised by the formation of a sinus in the cleft of the buttocks. It most commonly affects males aged 16-30 years.
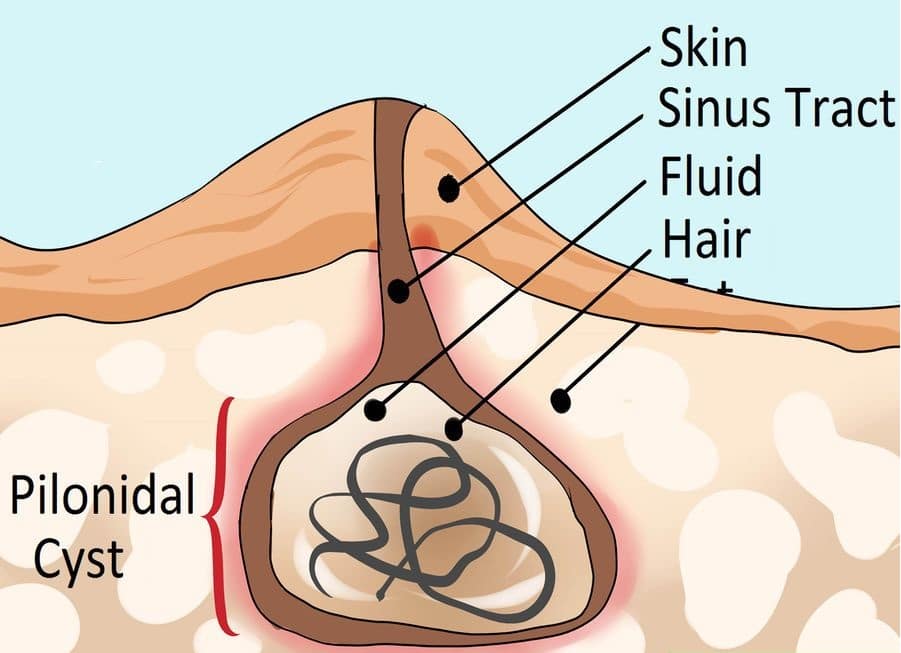
The most widely accepted theory for pilonidal sinus disease development begins with a hair follicle in the intergluteal cleft becoming infected or inflamed.
This inflammation obstructs the opening of the follicle, which extends inwards, forming a ‘pit’ (a characteristic feature of pilonidal sinus disease). A foreign body-type reaction may then lead to formation of a cavity, connected to the surface of the skin by an epithelialised sinus tract (Fig. 1).
These fluid-filled cavities (cysts) will often discharge serous fluid and can periodically become acutely infected to form a pilonidal abscess.
*The term pilonidal is derived from the Latin pilus (hair) and nidus (nest)
Risk Factors
Pilonidal sinus disease most commonly affects Caucasian males with coarse dark body hair. Classically, it is associated with those who sit for prolonged periods, such as lorry drivers or office workers.
Other associated factors are increased sweating, buttock friction, obesity, or poor hygiene. Typically, pilonidal disease does not occur after around 40yrs old.
Clinical Features
Pilonidal sinus disease most commonly presents as a discharging and intermittently painful sinus in the sacrococcygeal region (Fig. 2A). Discharge is typically episodic and of serous fluid, however this can become bloody or purulent discharge on occasion.
A pilonidal abscess can form when a pilonidal sinus becomes infected (Fig. 2B). This will present as a swollen and erythematous region. On examination, there will be a fluctuant and tender mass, as well as systemic features of infection.

Figure 2 (A) Pilonidal sinus opening B) Pilonidal abscess
Pilonidal Disease versus Perianal Disease
Pilonidal sinus disease is a disease affecting the natal cleft, whilst perianal fistula disease involves communication with the anal canal.
Pilonidal sinus disease lying very low (i.e. caudal) in the natal cleft however can be difficult to distinguish on clinical examination from perianal disease.
In such cases, proctoscopy and MRI imaging should be used for definitive assessment.
Investigation
The majority of cases of pilonidal disease can be diagnosed and managed without any further investigations required.
However, in cases of extensive or complex disease (e.g. multiple pit openings, previous surgery), an MRI of the sacrum can help delineate the extent of the disease, which will help in any operative planning required
Management
Pilonidal disease can be managed conservatively and does not always require surgical management. Conservative treatment of a pilonidal sinus involves removing any hair in the affected region (ideally with hair removal cream) and ensure the area is kept clean whenever possible.
For any pilonidal abscess that develops, these must be treated like any abscess and undergo incision and drainage +/-washout +/-packing. Elective surgery for the pilonidal sinus disease can then be performed at a later date if the patient remains symptomatic.
Elective Surgical Management
Treatment of chronic disease is the removal of the pilonidal sinus tract and multiple techniques have been described, depending on the severity of the disease.
For uncomplicated simple pilonidal disease, excision and laying open or excision and primary closure (e.g. a Karydakis procedure) of the tract or diseased area can be performed (Fig. 3).
For more advanced disease excision and advancement flaps (e.g. a V–Y flap) or excision and rotational flaps (e.g. Limberg flap) will be trialled. Newer approaches include endoscopic pilonidal sinus treatment (EPSiT), whereby the sinus tracts is explored with an endoscopic camera, cauterized, and the tract cleaned.
Risk of recurrence remains high, with some studies reporting 50% recurrence at 3 years.
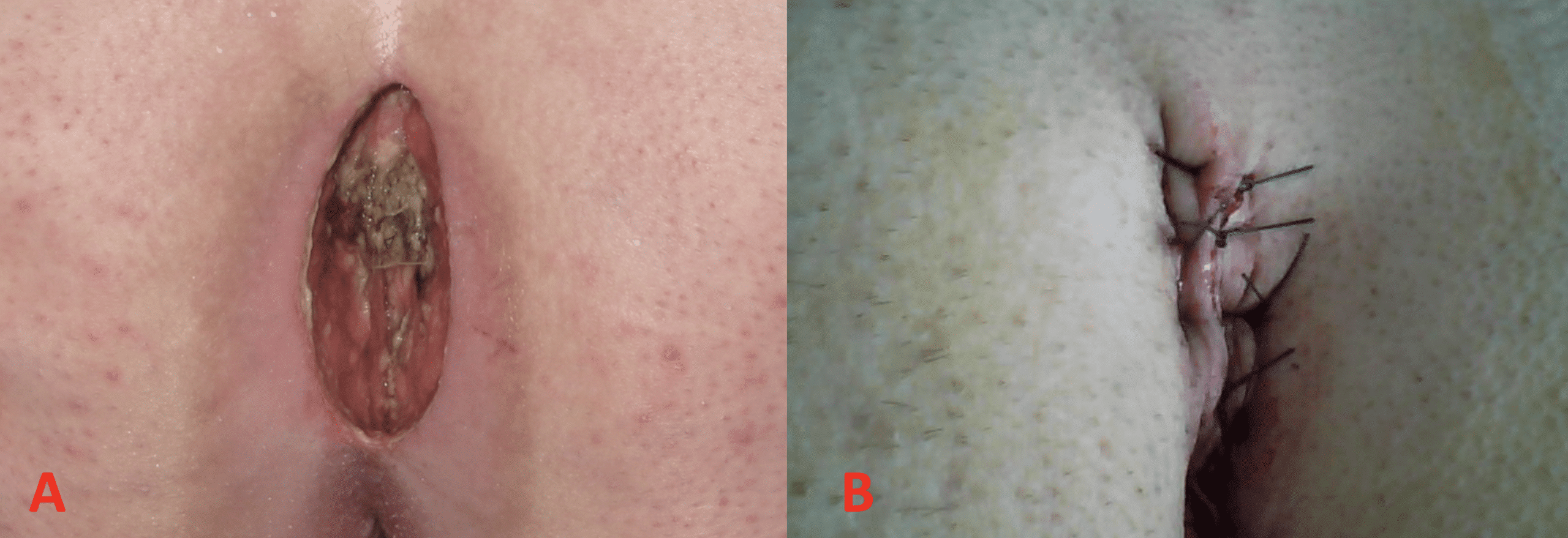
Figure 3 – Pilonidal Sinus Disease Surgery (A) Excision and Lay Open (B) Excision and Primary Closure
Key Points
- Pilonidal sinus disease occurs from the infection or inflammation of hair follicles in the cleft of the buttocks
- Cases commonly occur in those who may sit for prolonged periods, however the disease often does not present in those aged >40yrs
- Pilonidal abscesses require incision and drainage, whereas chronic disease needs to be treated with removal of the pilonidal sinus tract