Introduction
Tibial pilon fractures, also known as plafond fractures, are severe injuries affecting the distal tibia. They are caused by high energy axial loads as the tibial plafond is injured by the talus punching up into it.
Although these fractures account for <10% of lower limb injuries, their incidence is on the rise, mainly due to the increase in survivability from major road traffic accidents.
These fractures are characterised by articular impaction, severe comminution, and are often associated with considerable soft tissue injury. As such, they are complex injuries and often require specialist input.
Clinical Features
Patients will present with a history of trauma, usually that of a high-energy road traffic accident or a fall from a height. The patient will complain of severe ankle pain and an inability to weight-bear.
On examination, there may be an obvious ankle deformity, with associated significant swelling and bruising are common. In addition, skin blistering (fracture blisters) may occur over several hours.
It is very important to look for any evidence of an open fracture and for any signs of compartment syndrome, as these will significantly affect the management of these injuries.
Peripheral pulses should be assessed for vascular injury, whilst a peripheral nerve examination should be performed to test the superficial peroneal, deep peroneal, and tibial nerves.
Classification
The Ruedi and Allgower classification is a simple classification system used to describe the severity of pilon fractures:
- Type I – undisplaced intraarticular fracture
- Type II – displaced intraarticular fracture
- Type III – comminuted or impacted fracture
Differential Diagnosis
If sustained by a high-energy mechanism, it is important to look for other orthopaedic injuries. Commonly affected areas include the spine, pelvis, femur, tibial plateau or tibial shaft.
Investigations
Patients presenting following a major trauma should be investigated and managed as per the ATLS protocol.
Urgent bloods, including a coagulation and Group and Save, should be sent. Where a pathological cause is suspected, further work-up bloods, such as a serum calcium and myeloma screen, may be warranted.
Imaging
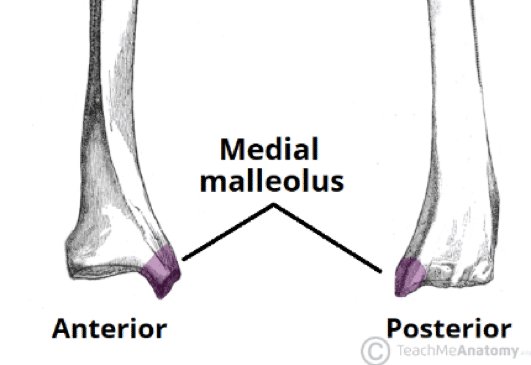
Plain film radiographs of the ankle should be requested (Fig. 2), with antero-posterior, lateral, and mortise views; full length views of the tibia and knee are also required. CT imaging is often subsequently required for further anatomical assessment and pre-operative planning
Management
Initial management of a pilon fracture involves realignment of the limb and application of a below-knee backslab. After which, a repeat neurovascular assessment and check plain film radiographs should be performed.
The limb must be elevated and monitored for compartment syndrome, and the patient kept nil by mouth with IV fluids in preparation for surgery.
Simple undisplaced pilon fractures are rare but may be treated non-operatively, particularly in elderly patients and patients to whom an operation is very high risk. However, as these injuries are intrinsically unstable, loss of reduction and subsequent malunion is common.
Surgical Management
The vast majority of pilon fractures are treated operatively, the timing of which depends on the degree of soft tissue involvement and the presence of any emergency complications (such as neurovascular injury).
Surgery aims to reconstruct the articular surface, restore the alignment of the ankle mortise, and protect the soft tissues around the ankle joint.
A staged approach is often the preferred management option, especially if significant soft tissue swelling. This involves the application of a temporary spanning external fixator followed by definitive fixation (ORIF) 7-14 days later once the soft tissues have had the opportunity to heal.
When definitive fixation does take place, it is best performed under traction, such as that provided by an external fixator. In other scenarios (e.g. in older patients or where definitive fixation has failed), fusion of the ankle with a hindfoot nail may be warranted.
Complications
Common complications following surgical repair include compartment syndrome, wound infection or dehiscence, delayed or non-union*, and post-traumatic arthritis.
*Commonly occurs in the metaphyseal region if there has been severe comminution, these injuries may require revision fixation and bone grafting
Key Points
- Tibial pilon fractures are severe injuries affecting the distal tibia, whereby the tibial plafond is injured by the talus punching up into it
- Patients will present following high-energy trauma, therefore concurrent injuries are common
- Check neurovascular status and for any evidence of an open fracture or compartment syndrome
- The vast majority of pilon fractures are treated operatively