Introduction
Urinary retention is as an inability to pass urine. It can be divided into either acute urinary retention or chronic urinary retention.
Acute urinary retention is defined as a new onset inability to pass urine*, which subsequently leads to pain and discomfort, with significant residual volumes.
The condition is most prevalent in older male patients, typically due to an enlarged prostate leading to bladder outflow obstruction, however there are a wide array of potential causes.
*Patients may pass small quantities of urine but have significant residual volumes and ongoing discomfort
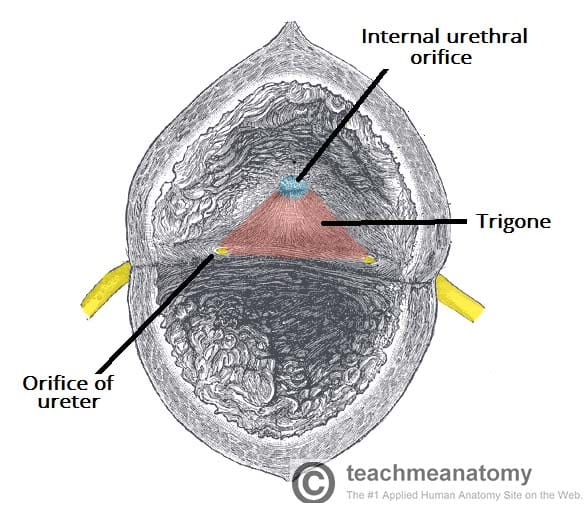
Figure 1 – The internal surface of the bladder, highlighting the trigone
Acute-On-Chronic Retention
Patients with chronic retention can also enter acute retention, either as an acute deterioration of the underlying pathology causing their chronic retention or a new aetiology superimposed on a background of chronic retention.
These patients will present often with minimal discomfort, despite very large residual volumes. They should be treated as per acute retention management, however may have much higher residual volumes than other acute retention patients, therefore more at risk to post-obstructive diuresis.
Aetiology
The most common cause in men is benign prostatic hyperplasia (BPH). Other common obstructive causes include urethral strictures or prostate cancer.
Urinary tract infections can cause the urethral sphincter to close, especially in those with already narrowed outflow tracts (e.g. BPH). Constipation can also cause acute retention, through compression on the urethra.
Severe pain can often cause patients to enter acute retention. Medications, such as anti-muscarinics or spinal or epidural anaesthesia, can affect innervation to the bladder, resulting in acute retention.
Neurological causes can include peripheral neuropathy, iatrogenic nerve damage during pelvic surgery, upper motor neurone disease (such as Multiple Sclerosis Parkinson’s disease), or DSD (detrusor sphincter dyssynergia)*.
*DSD is the lack of co-ordination of detrusor muscle contraction with urethral sphincter relaxation, leading to contraction against a closed sphincter, often seen with spinal cord pathology or traumatic injury
Clinical Features
Patients will present with acute suprapubic pain and an inability to micturate. This may be associated with symptoms suggestive of the predisposing cause, such as a urinary tract infection, recent change to medication, or worsening voiding LUTS.
On examination, the patient may have a palpably distended bladder, with suprapubic tenderness. Any associated fevers, rigors, or lethargy may suggest an infective cause. Ensure to perform a digital rectal examination, especially in older patients, to assess for any prostate enlargement or constipation.
Investigations
A post-void bedside bladder scan will show the volume of retained urine, helping to confirm the diagnosis.
All patients require routine bloods, especially FBC, CRP, and U&Es . Post-catheterisation, a CSU (Catheterised Specimen of Urine) should also be sent to assess for the presence of infection.
If there is a large volume of urine drained on catheterisation (>1000ml), then high pressure chronic retention (HPCR) should be ruled out*.
Patients with features of high-pressure retention will require an ultrasound scan of their urinary tract to assess for the presence of hydronephrosis. If this is confirmed, follow-up repeat imaging will be required in the subsequent weeks following treatment of the retention, to ensure its resolution.
*If the patient is found to have bilateral hydronephrosis or an acute kidney injury with no other cause then the patient is likely to have HPCR
Management
Patients will warrant immediate urethral catheterisation to resolve the retention. Ensure to measure the volume drained post-catheterisation.
The underlying causes should then be treated accordingly. For patients with an enlarged prostate, appropriate medication (typically Tamsulosin, an alpha receptor antagonist) should be started if suitable.
Ensure to check the CSU for any evidence of infection and treat with antibiotics if needed. Review the patient’s medication for any potential contributing causes and treat any constipation if present.
Definitive Management
Patients who have a large retention volume (>1000ml*) probably have a chronic element to their retention and would need to be monitored post-catheterisation for evidence of post-obstructive diuresis.
If patients have no evidence of renal impairment, a Trial WithOut Catheter (TWOC) will be attempted, whereby the catheter is removed after treatment of the cause. All men with a history of chronic lower urinary tract symptoms or a palpably large prostate should be started on an alpha-1 adrenoreceptor antagonist (e.g. tamsulosin) and can have their TWOC >72hrs after commencement.
If the patient voids successfully, with a minimal residual volume, the TWOC is considered successful, whilst if the patient re-enters retention, the patient will require re-catheterisation. Further TWOCs can be attempted (typically following a longer interval and preferably in a specialist TWOC clinic), however multiple failed attempts may warrant a long-term catheter, until definitive management can be arranged to treat the underlying cause.
Complications
Acute retention often presents early and if the cause is treated then few complications to the retention occur.
In patients with acute on chronic retention, acute kidney injury can occur, which can lead to chronic kidney injury if multiple episodes of retention leading to renal scarring.
Other complications include increased risk of urinary tract infections and renal stones due to urinary stasis.
Key Points
- Acute urinary retention is a new onset inability to pass urine, causing pain with significant residual volumes
- The most common cause is benign prostatic hyperplasia
- Patients require urgent catheterisation and ensure to check renal function, for evidence of high-pressure urinary retention
- Monitor for post-obstructive diuresis in those with large residual volumes


