Introduction
A glioma includes all primary brain tumours that originate from neuroepithelial glial cells (including ependymal cells, astrocytes, oligodendrocytes and astrocytes). Gliomas form the majority of all primary brain tumours, with both adults and children affected.
Low grade gliomas are the most common type of brain tumour in children, accounting for approximately 40% of childhood CNS tumours, whilst in adults, gliomas most commonly occur between 45-65yrs with an increasing incidence with age.
The main type of gliomas are ependymomas, astrocytomas, and oligodendrogliomas.
Classification
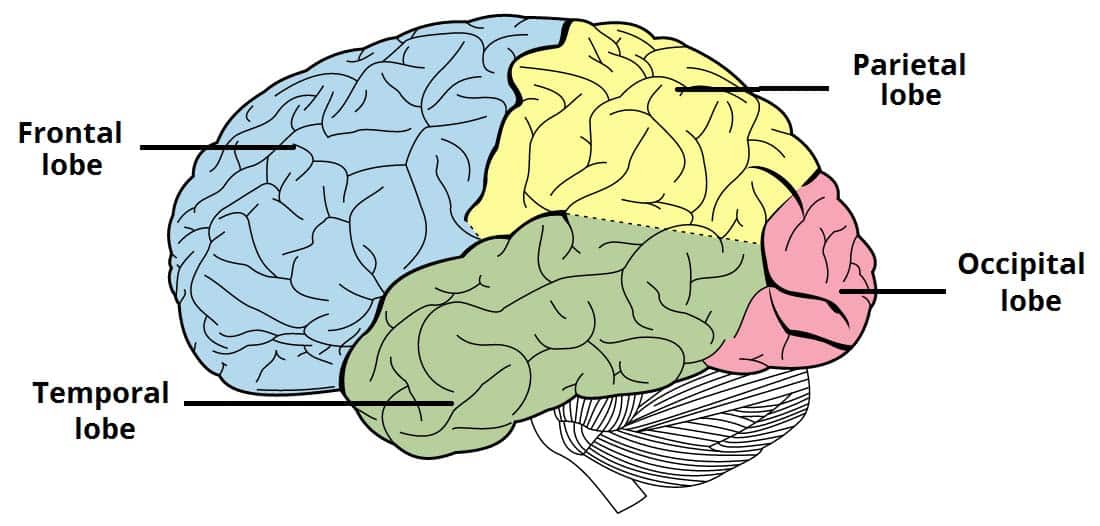
Gliomas can be classified by histological cell type (as above), location* (infratentorial vs supratentorial) or grade (grade I to IV).
Tumours that are well-differentiated and slow-growing are classified as low grade (Grade I and II), albeit can transform into higher grade tumours, and tend to have a better prognosis.
High grade tumours (Grade III and IV) are poorly differentiated and faster growing tumours that carry a worse prognosis. Examples include anaplastic astrocytomas (grade III) or glioblastoma multiforme (GBM, grade IV).
*Most gliomas in adults are suprtentorial whilst most gliomas in children and infratentorial
Clinical Features
Glioma presentation occurs as that of any space-occupying lesion. Common presenting features include seizures*, cranial nerve palsies or visual field defects, language dysfunction, or features of raised intracranial pressure.
*Seizures are the most common first symptom leading to a brain tumour diagnosis in adults and up to 60% of patients with brain tumours will experience at least one seizure
Differential Diagnosis
Potential differentials can be either neoplastic or non-neoplastic lesions. Neoplastic lesions include meningiomas, secondary metastasis, or lymphoma, whilst non-neoplastic causes of a mass lesion include infection (i.e. cerebral abscess) or infarction.
Investigations
CT head imaging with IV contrast is often the first line investigation performed. MRI imaging (Fig. 3) will often be used to further characterise and assess the lesion, with angiography performed to assess of tumour blood supply which can aid in any planned operative management.
A biopsy can be used to confirm the diagnosis, which can be achieved either through a stereotactic (burr hole) approach or through open exploration (craniotomy).
Management
Treatment options vary depending on the tumour grade. Treatment choice will also be affected by patient factors (e.g. age, co-morbidities, performance status) and treatment factors (e.g. probability of satisfactory excision or disease control, operative risks)
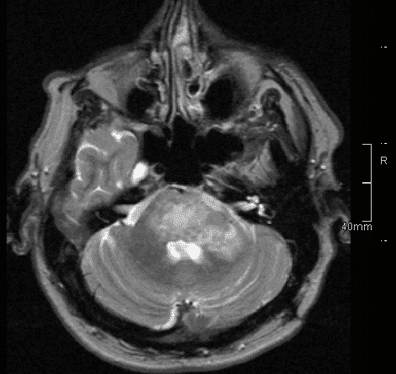
Figure 3 – MRI head showing a glioma within the brainstem
Low Grade Gliomas
In some cases of low grade gliomas, patients can be monitored with a watch and wait approach through radiological surveillance. Patients will have regular MRI scans to monitor tumour growth, however around 50% patients in this group will need debulking surgery within a few years of monitoring.
Those requiring surgery can undergo either a total or partial tumour debulking, attempting to remove as much neoplastic tissue as possible and relieve symptoms. Repeat procedures can often be required if not all tumour is excised.
Radiotherapy can be given after surgery especially in cases where there is tumour tissue left behind. Chemotherapy is growing in use, with its use now supported in cases with certain gene mutations are present (e.g. 1p19q)
High Grade Gliomas
Surgical intervention, either through total or partial decompressive tumour debulking, is the mainstay of treatment for high grade. Whilst this can be curative, symptomatic relief alone by reduction of tumour mass may also be required.
Histological samples of the tumour can also be obtained, helping to confirm the diagnosis and also guide further treatment.
Both radiotherapy and chemotherapy can have a role, both curative and palliative, in the treatment of high-grade gliomas. With radiotherapy, both conventional fractionated therapy or stereotactic radiotherapy can be employed; with chemotherapy, there is an established role for alkylating agents, such as temozolomide, post-operatively in patients who were previously fit and well.
Prognosis
Prognosis is mainly dependent on grade, as low grade gliomas have a median survival 15-16 years whereas high grade gliomas have a median survival 15-18 months (or less than 12 months without treatment).
Key Points
- A glioma is a primary brain tumour that originate from neuroepithelial glial cells
- They are classically classified into low-grade and high-grade tumours
- CT imaging of the head is often the first-line investigation for suspected cases
- Prognosis is mainly dependent on tumour grade