Introduction
Colorectal cancer is the fourth most common cancer in the UK, with around 40,000 new cases each year, and the second highest mortality of any cancer. It accounts for approximately 10% of all diagnosed cancers and cancer-related deaths worldwide, with the highest rates seen in the more developed countries.
Although like most cancers, the occurrence is strongly associated with age, it can occur in patients as young as 20yrs (with the incidence in young adults currently rising), especially in patients with inherited cancer syndromes.
In this article, we shall look at the risk factors, clinical features and management of colorectal cancer.
Aetiology
Colorectal cancers are most commonly adenocarcinomas, which originate from the epithelial cells lining the colon or rectum. Rarer types include lymphoma (~1%), carcinoid (<1%), and sarcoma (<1%).
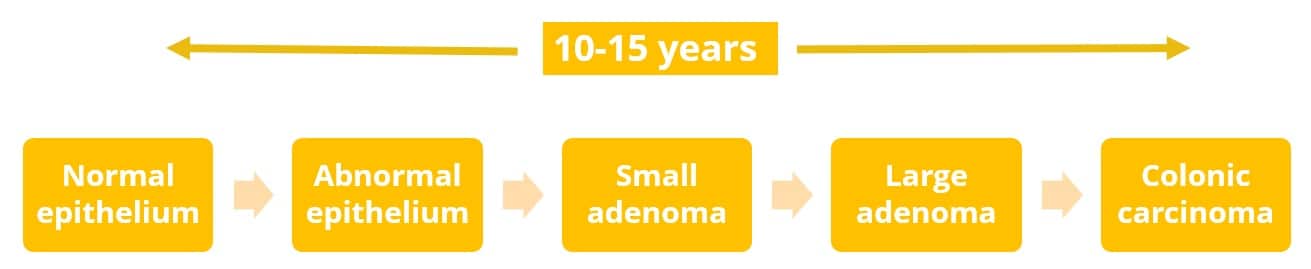
Most colorectal cancers develop via a progression of normal mucosa to colonic adenoma (colorectal ‘polyps’) to invasive adenocarcinoma (termed the “adenoma-carcinoma sequence”). Adenomas may be present for 10 years or more before becoming malignant; progression to adenocarcinoma occurs in approximately 5-10% of adenomas.
Certain genetic mutations have been implicated in predisposing individuals to colorectal cancer, most notably:
- Adenomatous polyposis coli (APC)
- A tumour suppressor gene, mutation of the APC gene results in growth of adenomatous tissue, such as Familial Adenomatous Polyposis (FAP)
- Hereditary nonpolyposis colorectal cancer (HNPCC)
- HNPCC is caused by mutations to DNA mismatch repair genes such as MLH1, MSH2, MSH6, PMS2, and EPCAM, leading to defects in DNA repair (this includes Lynch syndrome)
Risk Factors
Approximately 75% of colorectal cancers are sporadic, developing in people with no specific risk factors.
However, potential risk factors include increasing age, male gender, family history (positive family history is present in 10–20% of all patients with colorectal cancer), inflammatory bowel disease, low fibre diet, high processed meat intake, smoking, and excess alcohol intake.
Clinical Features
The common clinical features of bowel cancer include change in bowel habit, rectal bleeding, weight loss*, abdominal pain, and symptoms of (iron-deficiency) anaemia.
Classically, clinical features vary slightly depending on the location of the cancer:
- Right-sided colon cancers – abdominal pain, iron-deficiency anaemia, palpable mass in right iliac fossa, often present late
- Left-sided colon cancers – rectal bleeding, change in bowel habit, tenesmus, palpable mass in left iliac fossa or on PR exam
In the UK, NICE guidance recommends that patients should be referred for urgent investigation of suspected bowel cancer if:
- ≥40yrs with unexplained weight loss and abdominal pain
- ≥50yrs with unexplained rectal bleeding
- ≥60yrs with iron‑deficiency anaemia or change in bowel habit
- Positive faecal immunochemical test (FIT)
*As opposed to upper GI malignancies, progressive weight loss is usually only present in colorectal cancer cases with associated metastasis (or rarely in sub-acute bowel obstruction)
Differential Diagnosis
The symptoms associated with colorectal cancer can have a variety of possible diagnoses, however the main differentials to consider:
- Inflammatory bowel disease – The average age of onset of inflammatory bowel disease is younger (20-40yrs) than with colorectal cancer and typically presents with diarrhoea containing blood and mucus
- Haemorrhoids – Bright red rectal bleeding on the pan or surface of the stool, but rarely presents with abdominal discomfort or pain, altered bowel habits, or weight loss
Colorectal Cancer Screening
In England and Wales, screening is offered every 2 years to men and women aged 60-75 years. For most of the UK, a faecal immunochemistry test (FIT) is used, superseding the previous faecal occult test, which utilises antibodies against human haemoglobin to detect blood in faeces.
If any of the samples are positive, patients are offered an appointment with a specialist nurse and further investigation via colonoscopy. Since its introduction in 2006, the NHS Bowel Cancer Screening Programme has increased detection of colorectal cancer in people aged 60-69 by 11%.
Investigations
Laboratory tests
Routine bloods should be performed for all suspected cases. A full blood count (FBC) may show a microcytic anaemia (an iron-deficiency anaemia), as well as LFTs and clotting.
The tumour marker Carcinoembryonic Antigen (CEA)* should not be used as a diagnostic test, due to poor sensitivity and specificity, however it is used to monitor disease progression and should be conducted both pre- and post-treatment, monitoring for recurrence.
*An elevated baseline CEA is associated with worse prognosis
Imaging
The gold standard for diagnosis of colorectal cancer is via colonoscopy with biopsy. If a colonoscopy is not suitable for the patient, such as from frailty, co-morbidities, or intolerance, CT colonography can be performed for initial diagnosis (however, if any abnormalities are found, further treatment will need to be guided by a tissue biopsy)
Once the diagnosis is made, several other investigations are required (primarily for staging):
- CT scan (Chest/Abdomen/Pelvis) to look for distant metastases and local invasion
- MRI rectum (for rectal cancers only) to assess the depth of invasion and potential need for pre-operative chemotherapy
- Endo-anal ultrasound (for early rectal cancers, T1 or T2 only) to assess suitability for trans-anal resection

Figure 2 – Endoscopic image of colorectal adenocarcinoma.
Biopsy samples being sent for histology will be assessed using TNM staging, histological subtyping, grading, and assessment of lymphatic, perineural, and venous invasion. Increasingly, samples are also routinely being assessed for varying tumour-based markers (including mismatch-repair testing), to aid in the identification of Lynch syndrome and to optimise potential chemotherapy regimes.
Dukes’ Staging
Like many cancers, colorectal cancer is staged according to the TNM system. This stages the cancer according to the depth the tumour invades the bowel wall (T stage), the extent of spread to local lymph nodes (N stage), and whether or not there are distant metastasis (M stage).
Whilst the Duke’s staging system has now been largely superseded, it is still used at some centres for additional staging detail.
| Stage | Description | 5 Year Survival |
| A | Confined beneath the muscularis propria | 90% |
| B | Extension through the muscularis propria | 65% |
| C | Involvement of regional lymph nodes | 30% |
| D | Distant metastasis | <10% |
Management
All patients should be discussed with the multidisciplinary team (MDT). The only definitive curative option is surgery*, although chemotherapy and radiotherapy have an important role as neoadjuvant and adjuvant* treatments, alongside their role in palliation.
*A small proportion of early cancers (for T1 cancers) can be suitable for endoscopic resection techniques, such as en-bloc endoscopic mucosal resection or endoscopic submucosal dissection, however such techniques require substantial technical skills and expertise
Surgical
Surgery is the mainstay of curative management for localised bowel cancer. The general plan in most surgical management plans is suitable regional colectomy, to ensure the removal of the primary tumour with adequate margins and lymphatic drainage, followed either by primary anastomosis or formation of a stoma:
- Right Hemicolectomy or Extended Right Hemicolectomy
- The surgical approach for caecal tumours or ascending colon tumours, with the extended option performed for any transverse colon tumours. During the procedure the ileocolic, right colic, and right branch of the middle colic vessels (branches of the SMA) are divided and removed with their mesenteries
- Left Hemicolectomy
- The surgical approach for descending colon tumours. Similar to the right hemicolectomy, the left branch of the middle colic vessels (branch of SMA/SMV), the inferior mesenteric vein, and the left colic vessels (branches of the IMA/IMV) are divided and removed with their mesenteries
- Sigmoidcolectomy
- The surgical approach for sigmoid colon tumours. In this instance, the IMA is fully dissected out with the tumour in order to ensure adequate margins are obtained.
- Anterior Resection
- The surgical approach for high rectal tumours, typically if >5cm from the anus. This approach is favoured as leaves the rectal sphincter intact if an anastomosis is performed (unlike AP resections). Often a defunctioning loop ileostomy is performed to protect the anastomosis and reduce complications in the event of an anastomotic leak, which can then be reversed electively four to six months later
- Abdominoperineal (AP) Resection
- The surgical approach for low rectal tumours, typically <5cm from the anus. This technique involves excision of the distal colon, rectum and anal sphincters, resulting in a permanent colostomy
*Elective colectomies are often performed laparoscopically/robotically, as this offers faster recovery times, reduced surgical site infection risk, and reduced post-operative pain, with no difference in disease recurrence or overall survival rates when compared to open surgery
- Hartmann’s Procedure
- This procedure is used in emergency bowel surgery, such as bowel obstruction or perforation. This involves a complete resection of the recto-sigmoid colon with the formation of an end colostomy and the closure of the rectal stump (Fig. 3)
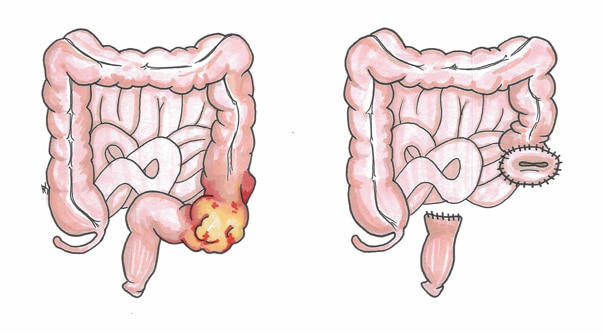
Figure 3 – A Hartmann’s Procedure, whereby the affected area of colon is resected, with the formation of an end colostomy and the closure of the rectal stump
Colorectal cancer presenting with bowel obstruction can be relieved by either a decompressing colostomy or endoscopic stenting, after which staging and patient status can be optimised
Chemotherapy
Chemotherapy is indicated typically in patients with advanced disease (adjuvant chemotherapy in Dukes’ C colorectal cancer has been found to reduce mortality by 25%). Systemic therapy for metastatic colorectal cancer is tailored with patient-specific and disease-specific predictive markers.
An example chemotherapy regime for patients with metastatic colorectal cancer is FOLFOX, comprised of Folinic acid, Fluorouracil (5-FU), and Oxaliplatin, which has been demonstrated to significantly improvement in 3-year disease-free survival for patients with advanced colon cancer.
Newer biologic or immunotherapy agents are being developed and utilised with increasing success.
Radiotherapy
Radiotherapy can be used in rectal cancer (it is rarely given in colon cancer due to the risk of damage to the small bowel), most often as neo-adjuvant treatment, and can be given alongside chemotherapy.
It is of particular use in patients with rectal cancers which look on MRI to have a “threatened” circumferential resection (i.e. within 1mm). They can undergo pre-operative long-course chemo-radiotherapy to shrink the tumour, thereby increasing the chance of complete resection and cure; time interval to surgery is then approximately 8-10 weeks.
Due to certain cases achieving complete response with chemo-radiotherapy, some patients with rectal cancer will opt for a rectal preserving treatment approaches, where a “watch-and-wait” strategy is employed with the omission of radical surgery and close surveillance.
Palliative Care
Very advanced colorectal cancers will be managed palliatively, focusing on reducing cancer growth and ensuring adequate symptom control.
Key Points
- Key symptoms of colorectal cancer are change in bowel habit and rectal bleeding
- Age, family history, and diet are important risk factors for developing colorectal cancer
- Gold-standard diagnosis is made via colonoscopy with biopsy
- CEA is only useful in monitoring treatment efficacy and disease recurrence, not to aid diagnosis
- Surgical resection remains the only definitive cure