This article is for educational purposes only. It should not be used as a template for consenting patients. The person obtaining consent should have clear knowledge of the procedure and the potential risks and complications. Always refer to your local or national guidelines, and the applicable and appropriate law in your jurisdiction governing patient consent.
Overview of Procedure
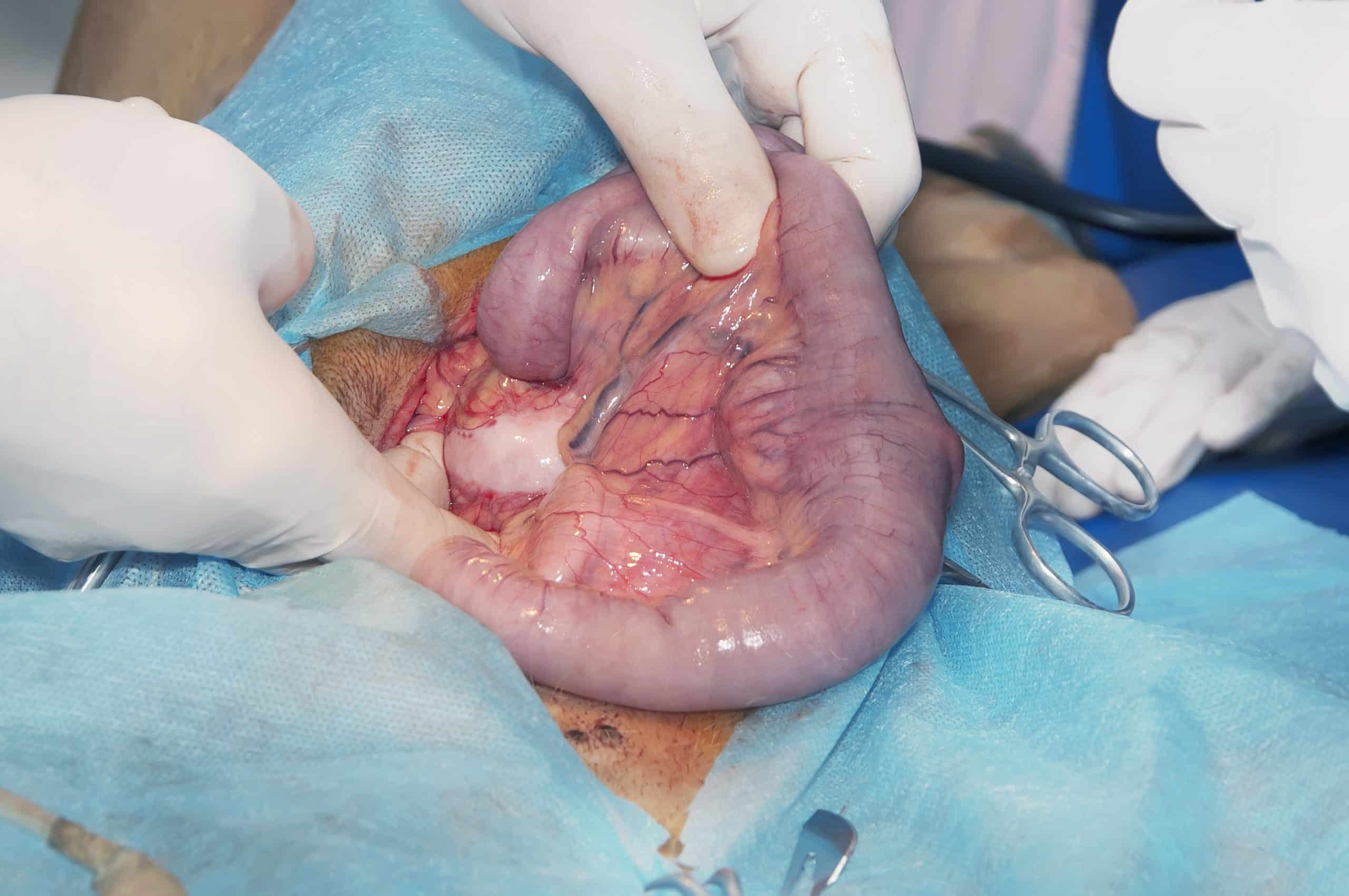
Small bowel resection is the surgical removal of a segment of the small bowel. These can be performed either open or laparoscopic, depending on the exact pathology, location of the pathology, patient co-morbidities, and urgency of the procedure.
Small bowel resections can be performed electively or as an emergency. Often the bowel can be re-joined with a primary anastomosis, however if deemed unsafe, the patient can be left with either a stoma (end or loop) or the bowel ends left closed off and a relook operation planned for a later date.
A small bowel resection is indicated in a number of conditions, including bowel perforation, bowel obstruction, ischaemic bowel, inflammatory bowel disease, small bowel malignancy, or fistulating disease. Infrequently, a defunctioning (proximal) stoma may also be required during the procedure.
Complications
Intra-Operative
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Bleeding | Ensure meticulous haemostasis during the procedure | |
| Damage to local structures | Caution when entering abdomen and performing any dissection | |
| Anaesthetic risks | Includes damage to the teeth, throat and larynx, reaction to medications, nausea and vomiting, cardiovascular and respiratory complications. | Forms part of anaesthetic pre-assessment |
Early
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Pain | Optimal post-operative analgesia, including epidurals or rectus sheath catheters | |
| Infection | Includes both wound infections and intra-abdominal collections | Intravenous antibiotics at induction, minimisation of faecal contamination during procedure, wound irrigation at closure |
| Anastomotic leak | Leak of intraluminal contents into the abdominal cavity through the anastomosis | Good blood supply at the anastomosis, not under tension |
| Ileus | Minimise contamination and bowel handling, correct any electrolyte abnormalities post-operatively | |
| Scarring | Use of laparoscopic surgery if possible to result in a smaller scar | |
| Re-operation | Any complication may result in the return to theatre in the immediate post-operative period | |
| DVT or PE, Myocardial Infarction, Stroke, or Mortality | Adequate pre-optimisation and anaesthetic assessment, peri-operative prophylactic LMWH, high-dependency level care post-operatively |
Late
| Complication | Description of Complication | Potential Ways to Reduce Risk |
| Adhesions | Attempt laparoscopic approach if possible, avoid excess tissue disruption | |
| Stoma complications | Includes stoma retraction, prolapse, or high stoma output, if a stoma is formed | |
| Hernia | Ensure fascia is closed tightly, using a small bites technique | |
| Short gut syndrome | If too much bowel has been resected, there becomes an impact on the absorption capacity of the bowel | Minimise distance of small bowel resected where safe to do so |