Introduction
Stridor is the noise made by turbulent flow of air being forced through narrowed upper airways.
The characteristic sound and associated features are seen when there is stenosis in the supraglottic, glottic, subglottic, or tracheal level*. Importantly, stridor is a symptom, not a diagnosis, thus further investigation is warranted to identify the underlying cause.
The timing of stridor during inspiration-expiration phases can be used to identify the likely level of airway obstruction (Table 1).
*Any obstruction above those levels will cause a stertor sound and obstruction at the level of the bronchi or below will cause a wheeze
| Inspiratory | Expiratory | |
| Supraglottic | X | |
| Glottic | X | X |
| Subglottic | X | X |
| Tracheal | X |
Table 1 – Phases of stridor to identify level of airway obstruction
Causes
Causes of stridor can be divided into acute and chronic, with incidence of each condition varying significantly with age
- Acute stridor – Foreign Body Inhalation, Epiglottitis, Laryngotracheobronchitis (Croup), Laryngitis, Anaphylaxis, and Neck Space Abscess
- Chronic stridor – Laryngomalacia, Subglottic Stenosis*, Vocal Cord Paralysis, Subglottic Haemangioma, Respiratory Papillomatosis, Macroglossia or micrognathia, and Malignancy
*Most commonly seen secondary to prolonged intubation
Bernoulli Principle
The Bernoulli principle states that an increase in the velocity of any fluid as it passes through a tube will cause a decrease in the linear pressure on the tube walls.
In cases of stridor, as the airway begins to narrow and the velocity of air flow at the narrowing subsequently increases, the linear pressure exerted will decrease and causes a collapse of the airway, resulting in the transmitted airway sounds.
Differential Diagnosis
The main differentials to consider in a case of stridor are:
- Stertor – a low-pitched snoring sound, resulting from stenosis between the nasopharynx to supraglottic regions
- Wheeze – a polyphonic expiratory airway sound, caused by lower airway narrowing
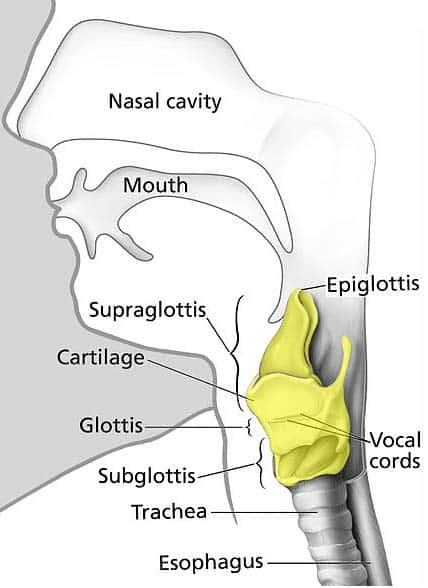
Figure 1 – Anatomical position of the larynx, continuous with the trachea inferiorly and the pharynx superiorly
Stridor itself is a red flag sign and investigation and management must be instigated urgently. Potentially more concerning is when the volume of the stridor sound decreases, as that can mean the patient is becoming tired and less air is being shifted by the lungs.
Important signs to assess for in all cases of stridor include torticollis and trismus, inability to swallow and drooling, absence of a cough, cyanosis, evidence of systemic infection, or poor response to initial management.
Investigations and Management
In most emergency situations, the diagnosis is clinical and initial management steps should be initiated to secure the airway before the results of the investigations are back. Definitive management steps will then vary between the underlying causes.
For non-emergency or chronic cases, visualisation of the upper airway will normally be done via fibreoptic nasal endoscopy* (Fig. 2), as a quick and minimally invasive means to differentiate where the pathology lies.
Further imaging studies, such as CT imaging, can be used in the case of abscess or malignancy, whilst bronchoscopy can be used if visualisation below the vocal cords is warranted, such as suspected subglottic stenosis.
*Any form of airway examination should be avoided in cases of suspected epiglottitis or croup, especially in children, as this can predispose to sudden airway closure
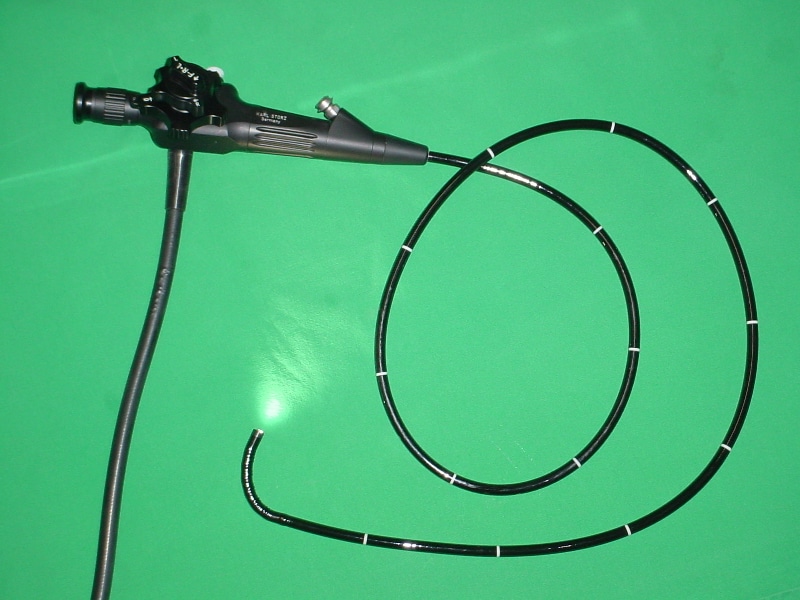
Figure 2 – A nasal endoscope, used to assess many cases of stridor
Acute Management
For acute causes that require urgent management, initial steps of securing the airway should involve:
- Stabilise the patient, start high-flow oxygen, and alert suitable senior specialists(ENT and / or anaesthetics)
- Try to suction secretionsor clear any foreign body from airway if obvious or visible
- Give adrenalineor steroids (IV or inhaled), as necessary
- Take blood tests, including an arterial blood gas or blood cultures if indicated
In emergency situations, be prepared to perform or assist with an emergency cricothyroidotomy or intubation
Epiglottitis
Epiglottitis is inflammation of the epiglottis and surrounding tissues, most commonly caused by H. Influenzae type B infections. The inflammation leads to narrowing of the airway and produces a characteristic high-pitched stridor.
Whilst it typically affects children between 2-7 years, vaccination against H. Influenzae* in many developed countries has dramatically reduced the incidence of acute epiglottitis. The incidence of the condition is still high in countries where the vaccine is not part of the routine vaccination
*Other causes include S. Pneumoniae, S. Pyogenes, P. Aeruginosa, or HSV
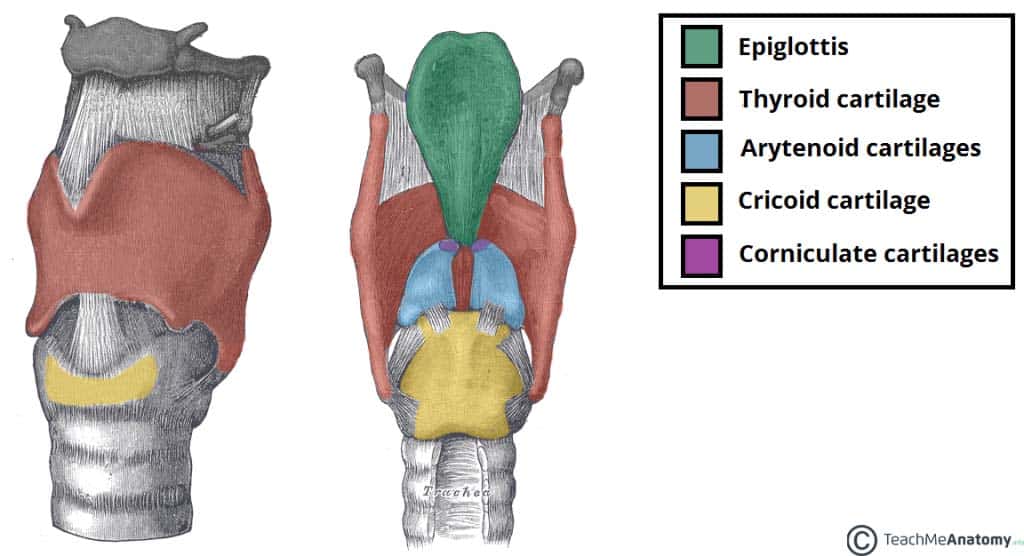
Figure 3 – Position of the epiglottis in relation to the laryngeal cartilages.
Clinical Features
Patients will initially present with a sore throat, a fever, and dyspnoea, characteristically in the absence of a cough. Late signs of the condition if left untreated include drooling, dysphagia, and stridor.
The patient will look unwell and is classically seen, in late stages on the disease, sitting in the tripod position (to allow gravity to assist in keeping the airway open).
Investigation and Management
All cases of epiglottitis need urgent assessment by senior anaesthetist or ENT surgeon, in a HDU or ICU setting (the airway should not be examined without such support due to the high risk of airway narrowing). When epiglottitis is suspected, do your best to not upset the child by examinations as this further increase the risk of airway collapse.
Nebulised adrenaline and IV dexamethasone should be started in all suspected cases. Blood and throat cultures should be taken and IV broad-spectrum antibiotics should be given, alongside analgesia and IV fluids. However, avoid inserting a cannula in a child as that will cause further distress. Once the patient is intubated, then the IV medications can be commenced.
Most cases are a clinical diagnosis, yet once initial management steps are in place, an Examination Under Anaesthesia (EUA) and intubation in theatre is required; fibreoptic nasal endoscopy can be attempted in an attempt to visual the airway to confirm the diagnosis (Fig. 4). Throat cultures can then be taken for MC&S.
Patients should be kept on intravenous antibiotics and steroids until the condition starts to improve. Close contacts of the patient who have not been vaccinated should be given appropriate antibiotic prophylaxis.
Laryngotracheobronchitis
Laryngotracheobronchitis (also known as croup) is inflammation of the larynx, trachea, and bronchus, including the vocal cords. Most commonly caused by a viral infection, the condition produces a characteristic barking cough, mostly affecting infants and children from 6 months to 2 years.
Croup is more common in colder months and most patients can be managed in the outpatient setting and only few require hospitalisation (only 2% of hospitalised patients will eventually require intubation).
Prognosis of croup is excellent, with the majority of cases completely recovering, yet potential complications include secondary infection (such as bacterial tracheitis) or dehydration (secondary to poor oral intake).
The cause of croup in 95% of cases is viral infection, common organisms including parainfluenza, influenza, RSV, and rhinovirus.
Clinical Features
Croup is a self-limiting illness, becoming worse within 48 hours and then gradually improving. It is typically preceded by an upper respiratory infection, before developing into dyspnoea and a characteristic barking cough, with potential fever. Symptoms are usually worse at night.
Croup Severity Grading
Severity of croup can be graded dependent on increasing clinical features, all having stridor and a barking cough, yet worsening stages including:
- Grade 1: + Expiratory Stridor
- Grade 2: + Pulsus Paradoxus
- Grade 3: + Cyanosis or Reduced Cognition
Investigations
Most cases do not require any investigations and can be made as a clinical diagnosis. Any higher-grade cases may warrant initial blood tests (FBC and CRP) for inflammatory makers to confirm the diagnosis and viral swabs to determine the potential viral strain.
Management
According to NICE guidelines, all children with croup should receive single dose of oral dexamethasone (0.15mg/kg) to reduce the inflammation and symptoms. Pain and fever can be controlled with paracetamol and ibuprofen, as needed. In any cases of dehydration, IV fluids may be considered alongside supplementary oxygen.
In the presence of any of the following signs, hospital admission should be considered:
- Known structural upper airway obstruction, a history of severe croup, or immunocompromise
- Uncertain diagnosis
- An unwell child with inadequate oral intake
- Less than 6 months old
In hospital, inhaled corticosteroids can be given, alongside nebulised adrenaline, to decrease airway inflammation. In severe cases, intubation may be warranted.
Key Points
- Stridor is causes by air being forced through narrowed upper airways.
- Causes of stridor can be divided into acute and chronic, most notably include Epiglottitis and Croup.
- Acute cases of severe stridor should be managed in an HDU setting with specialist team involvement.
- For non-emergency / chronic cases, investigation can be done via fibreoptic nasal endoscopy and CT imaging

