Introduction
The “acute abdomen” is defined as sudden onset severe abdominal pain.
Within this, there are large number of possible causes, including serious and life-threatening conditions, and therefore a structured approach is essential to ensure appropriate triage and timely management.
Initial Assessment
Any initial assessment for a patient presenting with an acute abdomen needs to identify whether this patient is acutely or critically unwell, that may require immediate surgical intervention or urgent medical therapy.
A short assessment of clinical status can be made by a general look (the “end-of-bed-o-gram”) and their observations. Any unwell patient should be approached with an A to E assessment and be urgently resuscitated.
Once the patient is appropriately resuscitated, further history and examination can be elicited. This will help further tailor the next investigation and management steps.
Presentations Needing Urgent Intervention
Acute Bleeding
There are multiple causes of intra-abdominal bleeding, both intra-luminal and extra-luminal.
The most serious cause of intra-abdominal bleeding is often the ruptured abdominal aortic aneurysm, which requires swift referral to the vascular team and immediate surgical intervention.
Other causes of intra-abdominal bleeding may require either interventional radiology, endoscopic, or surgical intervention, such as ruptured ectopic pregnancy, bleeding peptic ulcer (Fig. 1), or traumatic injury.
If untreated, these patients will go into hypovolemic shock, with clinical features including tachycardia, looking pale and clammy, and hypotension (importantly, patients may not necessarily present with abdominal pain)
Whilst each pathology has its own nuanced approach, key features of management include ensuring blood products are made available (including the use of major haemorrhage protocol if required), resuscitation, and early investigation and intervention.

Figure 1 – Endoscopic image of a bleeding gastric ulcer, which requires urgent endoscopic intervention
Perforated Viscus
Patients who present with a perforated viscus will often be very unwell. There are multiple causes of gastrointestinal perforation, including peptic ulcer disease, untreated bowel obstruction (either small or large bowel), diverticular disease, or inflammatory bowel disease.
Perforations range from small contained perforations, such as a localised diverticular perforation, to large perforations with uncontained contamination causing four-quadrant peritonitis, such a perforated colorectal cancer:
- Patients with a localised perforation can often present with localised pain and peritonism, tachycardia, and pyrexia (however may not necessarily look unwell!)
- Patients with generalised peritonitis will often present with tachycardia (+/- hypotension), pyrexia, and a rigid abdomen (and will look unwell!)
These patients need urgent resuscitation and most require cross-sectional imaging*, prior to final management be decided.
*In cases where the patient is in extremis and hence not stable enough to undergo imaging, if there is strong clinical suspicion of an intraabdominal pathology amenable to surgical intervention, immediate exploration in theatre may be warranted
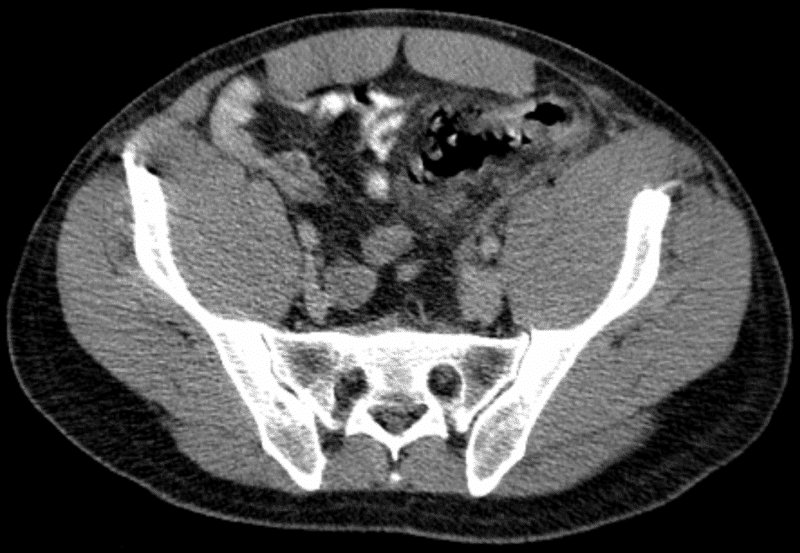
Figure 2 – CT scan showing a patient with perforated sigmoid diverticulitis
Ischaemic Bowel
Any patient who has severe pain out of proportion to the clinical signs should be assumed to have visceral ischaemia (typically ischaemic bowel) until proven otherwise.
Acute mesenteric ischaemia occurs when there is occlusion of a mesenteric vessel*, which will result in tissue infarction. Patients will typically present with severe and constant abdominal pain, however their examination may be otherwise unremarkable
Blood tests will often show a biochemical derangement (e.g. raised WCC and CRP) and a raised lactate and acidosis (although normal in approximately 25% of cases). Definitive diagnosis is made a CT scan with intravenous contrast (often requiring an arterial phase), and nearly always requires early surgical intervention (Fig. 3).
*This is different to ischaemic colitis, where reduced blood supply to the smaller vessels of the bowel can result is inflammation (but not necessarily causing any actual infarction of tissues)
Presentations Needing Further Investigation
Colic
Colic is an abdominal pain that crescendos to become very severe and then goes away completely, and is typical of a hollow viscus pathology.
The most common types of colic are biliary colic, ureteric colic, and bowel obstruction. They can be differentiated based on any triggers and timings with regards to the onset of pain, yet almost always further investigations are required
Once haemodynamically stable, patients should have routine blood tests and appropriate imaging, depending on the suspected pathology.
Peritonism
Peritonism (not peritonitis) refers to the localised inflammation of the peritoneum, usually due to inflammation of a viscus that then irritates the visceral (and subsequently parietal) peritoneum.
As such, patients will often report their pain starts in one place (irritation of the visceral peritoneum) before localising to one area (irritation of the parietal peritoneum) or becoming generalised.
The classic example of this is in acute appendicitis, where the pain will often migrate from the umbilical region (irritation of visceral peritoneum of the midgut) to the right iliac fossa (irritation of parietal peritoneum)
Differential Diagnoses
The location of abdominal pain is one useful feature that helps narrow the differential. These can be classified based upon quadrant or region affected (Fig. 4). A good history is usually key for discerning between the possible differentials.
It must be remembered to always consider extra-abdominal organs as the cause for abdominal pain, including cardiac, respiratory, gynaecological, or urological conditions.
Remember there are medical causes of abdominal pain to consider in patients presenting with abdominal pain, including diabetic ketoacidosis, atypical presentations of myocardial infarction, Addisonian crisis, or porphyria.
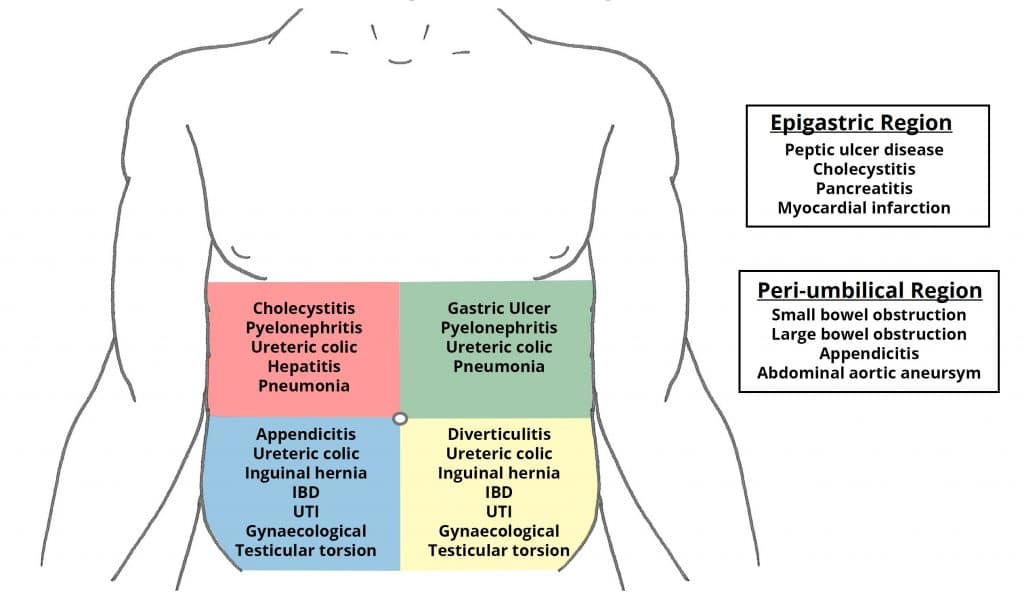
Figure 4 – Differential diagnoses for pain felt in the different regions of the abdomen.
Investigations
Initial Tests
The investigations in all cases of the acute abdomen share the same generic outline:
- Urine dipstick – for signs of infection or haematuria (and send for MC&S as required)
- Ensure a pregnancy test is performed for all women of reproductive age
- Arterial Blood Gas – useful in bleeding or acutely unwell patients, especially for the pH, pO2, pCO2, HCO3-, and lactate, for assessment of tissue hypoperfusion and a rapid haemoglobin level
- Routine bloods – FBC, U&Es, LFTs, CRP, amylase/lipase, and a G&S
- Ensure to crossmatch if blood products or urgent surgery required
- Electrocardiogram (ECG) – to assess for potential referred myocardial pain and for pre-operative work-up if any surgery required
Imaging
Following assessment, initial imaging may help to further help focus the diagnosis if still unclear:
- An erect chest plain film radiograph (eCXR), for evidence of free intra-abdominal air (Fig. 5) or a lower lobe lung pathology
- An abdominal plain film radiograph (AXR) may be useful in certain situations, for instance to investigate for recurrent volvulus
- Ultrasound imaging, most useful in assessing the renal tract (for hydronephrosis and cortico-medullary differentiation), biliary tree and liver (for gallstones, gallbladder thickening, or duct dilatation), and the uterus and adenexa (particularly if a transvaginal scan)
- CT imaging of the abdomen and pelvis, most useful in assessing for pathology in the gastrointestinal tract, such as bowel perforation
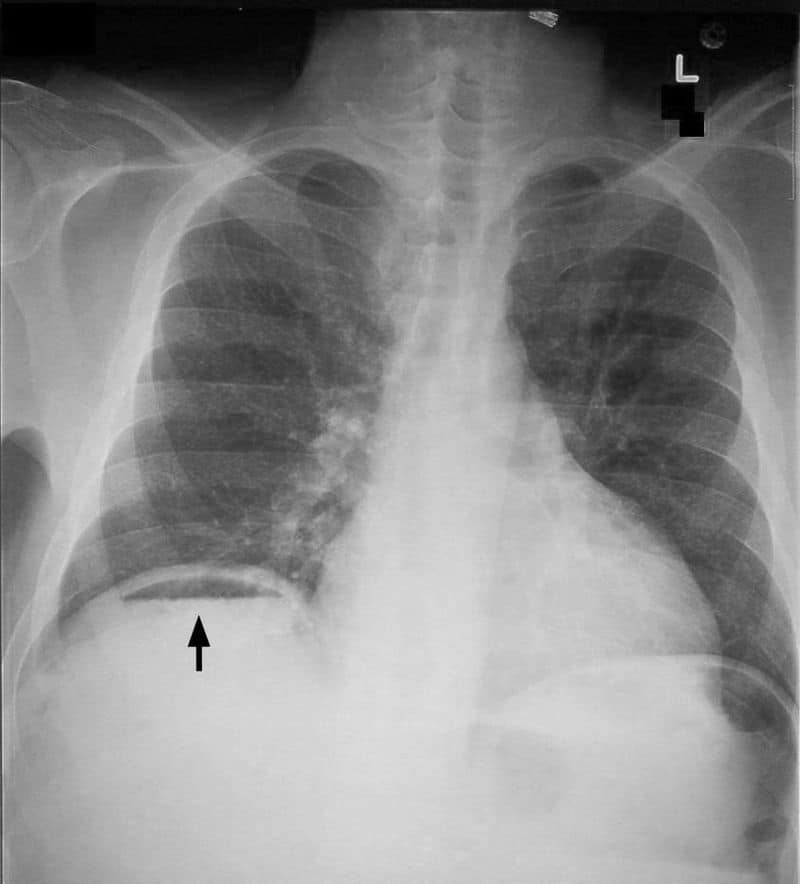
Figure 5 – An erect chest radiograph, showing free air under the right diaphragm (pneumoperitoneum)
Key Points
- The first decision when you first see any patient is “Are they critically unwell?”
- Wide array of pathologies that cause an acute abdomen, important to differentiate the urgent from non-urgent
- Routine bloods and initial imaging can help with aiding the diagnosis
- Management depends on the underlying cause, however ensure to start adequate resuscitation and early senior input

