Introduction
Acute respiratory distress syndrome (ARDS) is a form of acute lung injury, which is characterised by severe hypoxemia in the absence of a cardiogenic cause.
It occurs when there is inflammatory damage to the alveoli, which leads to pulmonary oedema, respiratory compromise, and ultimately acute respiratory failure.
Definition
The most up-to-date definition of acute respiratory distress syndrome is the Berlin Definition, which broadly consists of 4 key points:
- Acute onset within 7 days
- PaO2:FiO2 ratio <300 (with PEEP or CPAP >5cmH2O)
- Bilateral infiltrates on CXR
- Alveolar oedema not explained by fluid overload or cardiogenic causes
The degree of ARDS severity can be further defined, based on degree of hypoxemia via the PaO2:FiO2 ratio: Mild = 200-300mmHg, Moderate = 100-200mmHg, Severe ≤100mmHg.
Pathophysiology
The causes of acute respiratory distress syndrome can be divided into direct and indirect:
| Direct | Indirect |
|
|
Table 1 – Causes of ARDS
The pathophysiology of ARDS is complex, and can be divided into an exudative phase, a proliferative phase, and a fibrotic phase.
The exudative phase results in a diffuse alveolar damage (Fig. 1), initiated from the initial tissue injury (as per Table 1). During this phase, cytokines and various inflammatory mediators are all released that cause a direct alveolar and endothelial injury.
In the proliferative phase, there is progressive restoration of alveolar-capillary membrane integrity, by the fibroblasts and type-2 pneumocytes, in an attempt to normalise alveolar structure. New surfactant is also produced.
In the fibrotic phase, extensive fibrin deposition across the lungs can occur, leading to ‘scarring’ of the lung tissue. This can lead to substantial long-term morbidity, including need for long-term oxygen or even ventilation dependency.
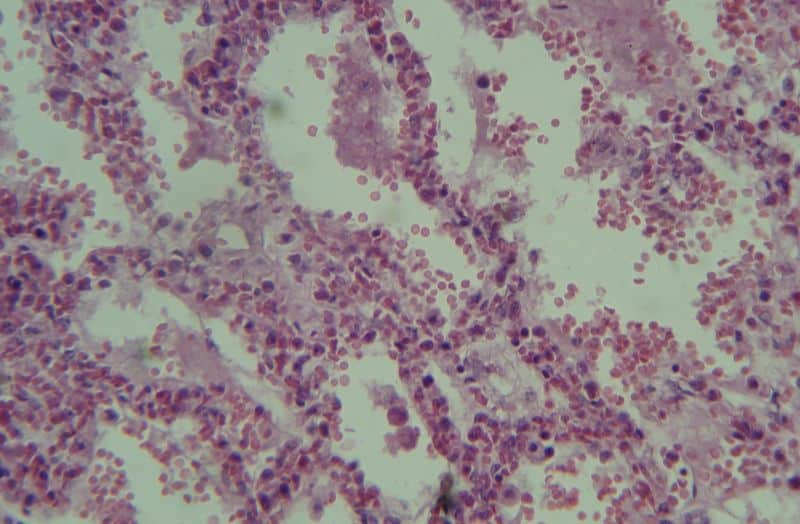
Figure 1 – The microscopic diffuse alveolar damage seen in acute respiratory distress syndrome
Clinical Features
Acute respiratory distress syndrome presents with (worsening) dyspnoea, usually in the presence of a related risk factor or underlying cause.
This then rapidly leads to hypoxia and tachypneoa, often with inspiratory crackles on auscultation. However, one of the most characteristic features to help make a diagnosis of ARDS is its acute onset (<7 days).
Differential Diagnosis
Multiple conditions present in a similar manner to ARDS, therefore ensuring the Berlin criteria are met for the diagnosis to be made is key.
Other differentials to consider include Congestive Heart Failure, Interstitial Lung Disease, Diffuse Alveolar Haemorrhage, and Drug-Induced Lung Injury.
Investigations
All patients with suspected ARDS should have the following basic investigations:
- Arterial blood gas, to assess degree of hypoxia
- Routine bloods
- Including FBC, U&Es, amylase, and CRP, which will help identify any evidence of infection, disease severity, and potential cause of ARDS
- Chest radiograph (CXR)
The CXR in a case of ARDS typically shows diffuse bilateral infiltrates (Fig. 2), similar to that of pulmonary oedema. A CT thorax scan may be required if the CXR is inconclusive. Echocardiography should also be performed to exclude a potential cardiogenic cause for the clinical picture.
The suspected underlying cause of the acute respiratory distress syndrome will determine which further investigations are then required (such as sputum cultures)
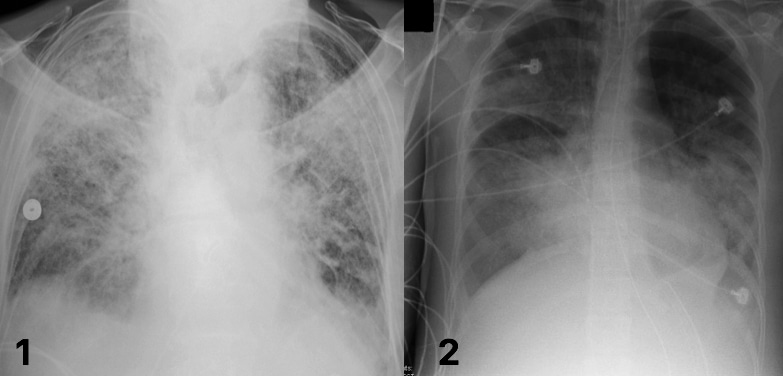
Figure 2 – Chest radiographs demonstrating extensive bilateral infiltrates in acute respiratory distress syndrome
Management
The management of acute respiratory distress syndrome is (i) supportive treatment with ventilation (ii) focused treatment of the underlying cause. It is highly likely that patients with ARDS will require early intubation and ITU admission for respiratory and circulatory support.
The specific goals of ITU management of ARDS are complex, focusing on limiting the inflammatory cascade and reducing alveolar injury. However, the main aspects of management* involve:
- Maintaining the minimum intravascular volume required to ensure adequate tissue perfusion, thus limiting excess oedema
- Lower tidal volumes used in ventilation, reducing shear forces from over-distension and ventilator-associated lung injury
- Positive end-expiratory pressure, splinting airways and avoids the damage caused by the cyclical opening of alveoli
Patients who remain severely hypoxic despite conventional therapy, Extra-Corporeal Membrane Oxygenation (ECMO) can be considered
*Proning patients has also been shown to improve oxygenation and CO2 clearance, therefore can be used in conjunction to the other ventilation measures
Pharmacological Treatment of ARDS
Pharmacological treatments of ARDS have in the past involved the use of artificial surfactant and corticosteroids, however are used less in modern practice.
Use of artificial surfactant can be effective in neonatal cases, however has yielded no advantage in adults, whilst the use of corticosteroids are not effective in the acute phase of ARDS (but may reduce ventilation days when used 7-14 days after onset).
Prognosis
Acute respiratory distress syndrome remains associated with a high mortality (around 40% in many centres), although it varies dependent on multiple factors.
Known prognostic factors include increasing age, number of co-morbidities, active malignancy, and liver disease. Even once discharged, around half of patients will have an inability to complete a 6-minute walk test.
Key Points
- Acute respiratory distress syndrome remains associated with a high mortality
- Its causes can be divided into either direct or indirect
- Management of ARDS comprises both of supportive treatment with ventilation and focused management of the underlying cause
