Introduction
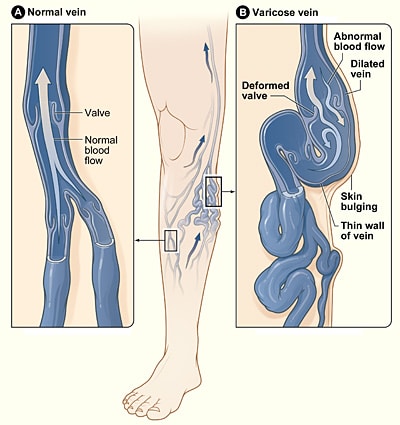
Varicose veins are tortuous dilated segments of vein associated with valvular incompetence.
They arise from incompetent valves, which permit blood flow from the deep venous system to the superficial venous system (mainly at the sapheno-femoral junction and sapheno-popliteal junction, but other perforating veins exist). This results in venous hypertension and subsequent dilatation of the superficial venous system (Fig. 1)
98% of varicose veins are primary idiopathic varicose veins. Secondary causes may include deep venous thrombosis, pelvic masses (e.g. pregnancy or uterine fibroids), or arteriovenous malformations (such as Klippel-Trenaunay Syndrome).
The Edinburgh Vein Study showed an age-adjusted prevalence rate for varicose veins of 39.7% in men and 32.2% in women, with around 40% of women affected during or after pregnancy. The risk of varicose veins increases every year by 1.9% in men and 2.6% in women.
Risk Factors
There are four major risk factors for the development of varicose veins:
- Prolonged standing
- Obesity
- Pregnancy
- Family history
Clinical Features
Patients with varicose veins will typically present initially with cosmetic issues*, reporting unsightly visible veins or discolouration of the skin
Worsening varicose veins may then cause aching or itching. Subsequent complications if left untreated can include skin changes (see below), thrombophlebitis, ulceration or bleeding (often presenting post-trauma).
On examination, varicosities will be present in the course of the great and / or short saphenous veins (Fig. 2). They can also present with clinical features of venous insufficiency, such as ulceration, varicose eczema, or haemosiderin deposition.
*In the UK, cosmetic issues alone does not qualify for treatment of varicose veins

Figure 2 – Varicose veins presenting on the posterior leg
Saphena Varix
A saphena varix is a dilatation of the saphenous vein at the saphenofemoral junction in the groin. As it displays a cough impulse, it is commonly mistaken for a femoral hernia; suspicion should be raised in any suspected femoral hernia if the patient has concurrent varicosities present in the rest of the limb. These can be best identified via duplex ultrasound and management is via high saphenous ligation.
Classification
A standardised reporting method for the clinical manifestations of varicose veins has been described by the CEAP Classification
|
Clinical Features |
| C0 -No visible or palpable signs of venous disease; C1 – Telangiectasias or reticular veins; C2 – Varicose veins (C2r – Recurrent varicose veins); C3 – Edema; C4 – Changes in skin and subcutaneous tissue secondary to CVD (C4a – Pigmentation or eczema, C4b – Lipodermatosclerosis or atrophie blanche, C4c – Corona phlebectatica); C5 – Healed; C6 – Active venous ulcer (C6r Recurrent active venous ulcer) |
|
aEtiology |
| Ep – Primary; Es – Secondary (Esi – Secondary intravenous, Ese – Secondary extravenous); Ec – Congenital; En – No cause identified |
|
Anatomical |
| As: Superficial veins, Ap: Perforating veins, Ad: Deep veins, An: no venous location identified |
|
Pathophysiology |
| Pr: Reflux, Po: Obstruction, Pr,o: Reflux and Obstruction, Pn: no venous pathophysiology identifiable |
Table 1 – The CEAP classification for the clinical manifestations of varicose veins
Investigations
Gold standard for varicose vein investigations is via duplex ultrasound, assessing for valve incompetence at the great or short saphenous veins and any perforators. Deep venous incompetence, venous occlusion (i.e. deep venous thrombosis), and venous stenosis must also be actively assessed for.
Management
Non-Invasive Treatments
Patient education is very important, such as avoiding prolonged standing, weight loss, and increase exercise (promotes calf muscle action).
Compression stockings should be used (ensure to check the patients ABPI prior to use) if interventional treatment is not appropriate; compression stockings act to prevent the complications of varicose veins but need to be worn lifelong
Any venous ulceration from deep venous incompetence generally requires compression therapy at 40mmHg pressure. This may be through four-layer bandaging, stockings, short stretch bandaging, or compression wraps, unless there is evidence of arterial insufficiency.
Varicose Veins and Concurrent DVT If a patient is identified to have a concurrent DVT, you cannot treat their superficial incompetence, due to the risk of worsening venous hypertension by removing further venous drainage from the leg. Consequently, any patient with varicose veins and deep venous thrombosis is typically offered non-surgical management. There may be the potential to offer intervention in the future when out of the acute phase.
Surgical Treatment
Patients with varicose veins should be referred to a vascular service if they meet the following criteria:
- Symptomatic primary or recurrent varicose veins
- Lower‑limb skin changes, such as pigmentation or eczema, thought to be caused by chronic venous insufficiency
- Superficial vein thrombosis (characterised by the appearance of hard, painful veins) with suspected venous incompetence
- A venous leg ulcer (a break in the skin below the knee that has not healed within 2 weeks)
The treatment options that are available include:
- Thermal ablation – involves heating the vein from inside (via radiofrequency or laser catheters), causing irreversible damage to the vein, resulting in fibrosis and closure of the vein lumen; this is done under ultrasound guidance and can be performed under local (or general) anaesthetic, and is the most common treatment method currently
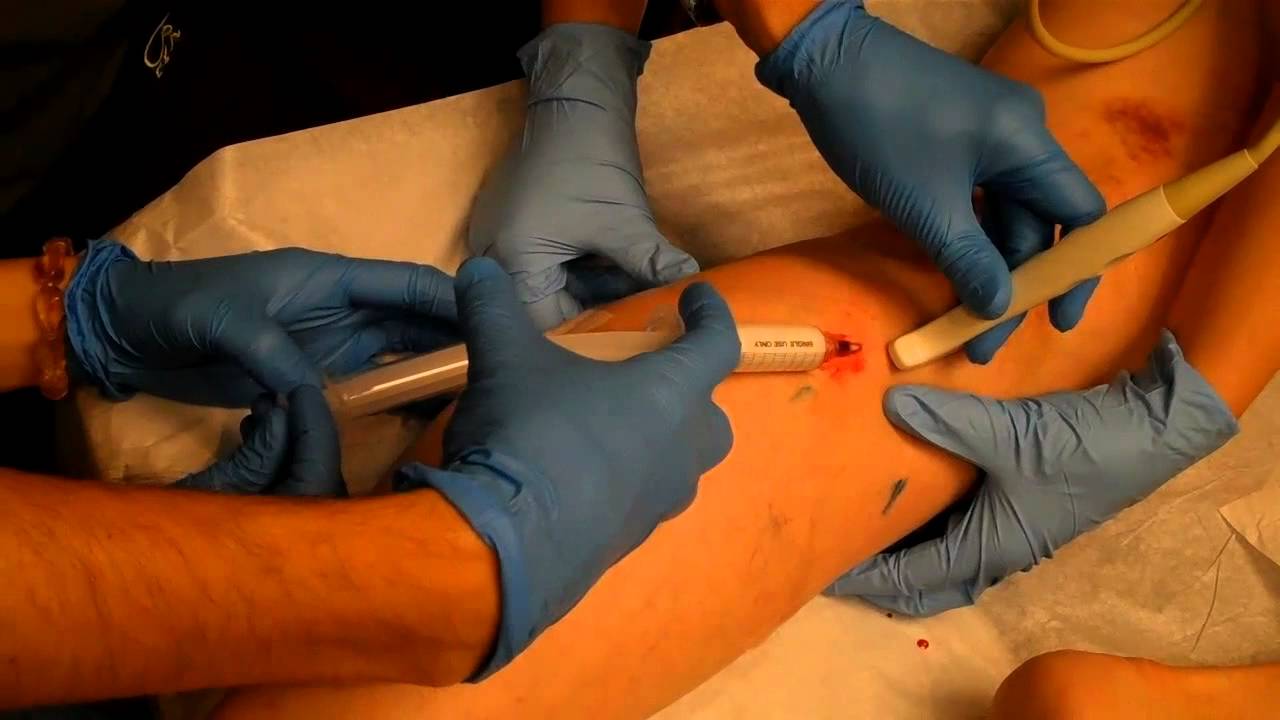
- Foam sclerotherapy – involves injecting a sclerosing (irritating) agent directly into the varicosed veins, causing an inflammatory response that closes off the vein (Fig. 3); this is done under ultrasound guidance to ensure the foam does not enter the deep venous system, however this method often only requires local anaesthetic
- Vein ligation, stripping, and avulsion – involves making an incision in the groin (or popliteal fossa) and identifying the responsible refluxing vein, before tying it off and stripping it away; whilst less commonly done as the primary procedure, avulsions may be performed under local anaesthetic alongside thermal ablation techniques
Complications
Untreated varicose veins will worsen over time and indeed many patients who have treated varicose veins often require re-intervention surgery, as there is a 50% recurrence rate at 10 years.
Whilst the complications will be specific for each procedure, typical complications seen post-operatively include haemorrhage, thrombophlebitis (important for foam or ablation treatments), deep vein thrombosis (important for any endovenous treatments), recurrence, and nerve damage (specifically saphenous or sural nerves).
Key Points
- Varicose veins are tortuous dilated segments of vein associated with valvular incompetence
- Risk factors include prolonged standing, obesity, pregnancy, and positive family history
- Most will simply be a cosmetic issue however can present with pain, aching, swelling, or itching
- Gold standard investigation is duplex ultrasound
- Management options in those that meet the criteria include vein ligation and stripping, foam sclerotherapy, and thermal ablation