Introduction
Breast surgery aims to remove breast cancer and assesses evidence of local (axillary) spread. Breast and axillary surgery allows assessment of tumour size, biology, and nodal spread more accurately than imaging and biopsy alone.
This helps to not only achieve disease control but provides information to guide any adjuvant treatment. Breast surgery aims to achieve effective oncological treatment whilst maintaining breast cosmesis and symmetry.
Surgical Treatments
Breast Conserving Surgery
Breast Conserving Surgery (BCS) is generally only suitable for patient with localised disease and no evidence of metastatic disease.
The foundation of BCS is wide local excision (WLE), which comprises removing the breast cancer with a cuff of healthy tissue around it. Breast conserving surgery can be considered when the size of the breast cancer is small relative to the breast size. As such, a wide local excision can be performed without significantly disrupting the breast shape (Fig. 1).
Techniques vary in complexity from incision placement directly over the area of disease, to approaches which hide scars beneath clothing, around the areola, or within the Infra mammary fold. More recently oncoplastic techniques (discussed below) can allow reshaping of the breast or transposition of local tissue flaps to ensure optimal cosmetic outcomes whilst still achieving oncological control.
Many breast cancers are clinically not palpable therefore must be localised prior to surgery, so as to target excision. Localisation techniques include image-guided guidewire or magseed insertion, which allow for more accurate surgery.

Figure 1 – Incision following a wide local excision for suspected breast malignancy
Mastectomy
A mastectomy entails removing the entirety of the breast tissue (in practical terms, approximately 95% of the breast tissue is removed). Mastectomies are indicated in cases of multifocal disease, high tumour:breast tissue ratio, disease recurrence, patient choice, or for risk-reduction.
Mastectomies can be performed with varying preservation of the breast skin envelope (and nipple). Whilst “simple mastectomies” involve excision of an area of skin overlying the breast to result in a flat cosmesis, skin-sparing (SSM) and nipple-sparing mastectomy (NSM) can also be performed. Both SSM and NSM allow for the preservation of a breast envelope so as to facilitate reconstruction.
Risk Reducing Mastectomy
A risk-reducing mastectomy is an operation to remove healthy breast tissue in order to reduce the risk of developing breast cancer.
Rsk-reducing mastectomies are only suitable for patients with a high risk of developing breast cancer and requires appropriate counseling to reach this difficult decision. In cases of suspected genetic risks, then patients are often referred to a genetic counsellor.
Factors conferring risk include:
- A strong family history of breast or ovarian cancer
- Testing positive for genetic mutations, such as BRCA1 or BRCA2, PTEN, or TP53 mutations
- Previous history of breast cancer
Axillary Surgery
Axillary surgery can be divided into Sentinel Lymph Node Biopsy (SLNB) and Axillary Node Clearance (ANC)
Sentinel Lymph Node Biopsy
Breast cancer will generally metastasise initially via the lymphatics, therefore a SLNB allows for the assessment of potential lymphatic spread.
SLNB involves removal of the sentinel lymph node, which is the first lymph node (or nodes) into which the breast drains. Sentinel lymph nodes are identifiable following injection of technetium-99 nanocolloid. This gamma emitting radioisotope maps to the lymph nodes via the lymphatics.
Radioactive nodes can the be identified intra-operatively using a gamma probe and analysed for cancer spread. Lymph node mapping methods can also utilise blue dye (which stains sentinel lymph nodes blue) or solutions containing superparamagnetic iron oxide particles, which can also be identified with a specialist probe.
Axillary Node Clearance
Axillary node clearance involves removing all nodes in the axilla. This is performed when nodal spread is confirmed on biopsy during initial investigations. It allows both staging the extent of axillary disease involvement (so as to guide adjuvant treatments) and controls or removes axillary disease.
ANC require meticulous dissection and preservation of key neurovascular structures within the axilla. Important structures include the axillary vein, the thoracodorsal pedicle, and the long thoracic nerve of Bell*. Additional risks of axillary node clearance include paraesthesia, seroma formation, and lymphedema in the upper limb (in 20-30%).
*The long thoracic nerve is responsible for motor innervation of the serratus anterior muscle and damage to this nerve causes winging of the scapula
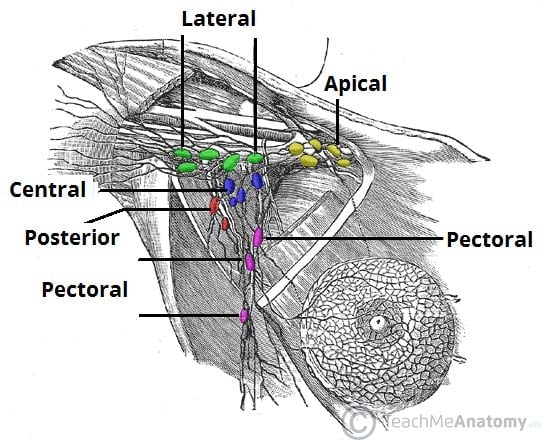
Figure 1 – The lymphatic drainage of the breast and associated axillary lymph nodes
Oncoplastic Management
Oncoplastic surgery has emerged as a means of reshaping breasts or replacing volume with local or distant autologous tissue, so as to replace volume in larger excisions which would previously have resulted in mastectomy.
Multiple flap reconstructive techniques are available (discussed below). Alternatively, a therapeutic mammoplasty may be considered in certain patient, which involves a WLE combined with breast reduction techniques. This technique is suited to larger ptotic breasts and results in a smaller uplifted breast.
Flap Reconstructive techniques
Local Flap Techniques
Local flap techniques involve the mobilisation of regional tissue to replace volume lost after wide local excision or mastectomy. These include the dermis and skin flaps perfused by local artery perforators, such as the lateral intercostal artery perforator (LICAP) or anterior intercostal artery perforator (AICAP).
A Latissimus Dorsi Flap involves mobilisation of the latissimus dorsi off its spinous processes insertions posteriorly so it can be transposed onto the chest wall anteriorly. This can be performed as a reconstructive option following mastectomy.
Free Flap Techniques
Free flap techniques can also be used for breast reconstruction. Deep Inferior Epigastric Perforator (DIEP) flaps can be used, which utilises tissue from the abdomen and its overlying skin to reconstruct the breast following mastectomy.
These tissues are harvested and their blood supply disconnected and anastamosed to chest wall vessels (classically the internal thoracic). This requires microsurgical expertise and is commonly performed by plastic surgical teams.
Key Points
- A wide array of surgical options are available for treatment of breast cancer
- Decisions for wide local excision versus mastectomy will be made depending on tumour size, location, size of breast, prior history of breast cancer, and patient preference
- Improvements in oncoplastic techniques have broadened the options for breast conservation and reduced the need for mastectomy
